Translate this page into:
A clinical study to ascertain the effectiveness of homoeopathic medicines in the treatment of scalp psoriasis
*Corresponding author: Dr. Rajitha K. Nair, Department of Repertory, Government Homoeopathic Medical College, Trivandrum, Kerala, India. rajithaknair@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Nair RK, Sasi AK. A clinical study to ascertain the effectiveness of homoeopathic medicines in the treatment of scalp psoriasis. J Intgr Stand Homoeopathy. 2023;6:95-101. doi: 10.25259/JISH_12_2023
Abstract
Objectives:
Psoriasis was recognised as a major non-communicable disease in the World Health Assembly decision WHA67 on 24 May 2014. One of the most typical locations for psoriasis manifestations is the scalp; this has a detrimental effect on the patient’s quality of life.
Materials and Methods:
Study participants were chosen from among patients who attended the psoriasis research outpatient clinic at the Government Homoeopathic Medical College Thiruvananthapuram, Kerala. With the help of a dermatologist, the patients were clinically identified and case documentation was completed using a standardised case record format. The gathered data were analysed using the Psoriasis Area and Severity Index (PASI) and Dermatology Life Quality Index (DLQI) following the administration of the homoeopathic medicine.
Results:
It is clear from the current study of 30 instances that by comparing the PASI scores and DLQI ratings for the area of psoriasis lesions on the scalp before and after therapy, the study’s overall effectiveness was determined. After the medication was administered, PASI scores and DLQI considerably reduced and patients reported an improvement in their quality of life.
Conclusion:
Homoeopathy can effectively treat scalp psoriasis. It most frequently affects the scalp, which has a detrimental effect on people’s quality of life. The proper treatment and limiting of impairments depend on early detection and intervention. In the current scenario, our statistical data depict that homoeopathy holds a pivotal role in the choice of various health systems for cost-effective and successful treatment of scalp psoriasis.
Keywords
Scalp psoriasis
Psoriasis area and severity index
Dermatology life quality index
Homoeopathy
INTRODUCTION
Psoriasis is a non-communicable, chronic skin condition that affects 1–3% of the general community.[1] Psoriasis, which has a prevalence that ranges from 0.09% to 11.43% worldwide, affects at least 100 million individuals. The disease has a chronic, remission- and exacerbation-prone trajectory. Psoriasis was recognised as a major non-communicable disease in the World Health Assembly decision WHA67 on 24 May 2014.[2] It frequently coexists with several comorbid diseases due to its systemic nature, including diabetes, hypertension, cancer and cardiovascular disease.[3]
Up to 80% of people with psoriasis have symptoms on their scalp, which is where the disease most frequently manifests. Scalp psoriasis has a detrimental effect on most patients’ quality of life. The patient may experience annoyance as well as itching, pain, bleeding and embarrassment that affect social contact and personal relationships.[4] Hairline psoriasis is challenging to cure. Administering medications incorrectly, which may cause facial itchiness, messy, time-consuming and cosmetically unappealing applications, as well as hair soiling, frequently causes improvements to be delayed and treatment duration to be extended.[5]
Younger people frequently get scalp lesions, which present patients with a major dilemma because the lesions and scaling are noticeable and cause them to feel stigmatised.[6] The typical scalp lesion is characterised by clearly defined erythematous plaques covered in scales that are silvery-white in colour. In psoriasis with scalp involvement, hair loss is less prevalent, although in the majority of these cases, scratching the lesions is likely to be the culprit. It is a well-known observation that scalp psoriasis that lasts for a longer time or is more severe tends to leave scars, which can lead to secondary scarring alopecia.[7] In a recent systematic review, the authors found that psoriasis is associated with many mental disorders such as eating disorders, sleep disorders, sexual disorders, substance abuse and dependence, psychosis, bipolar disorder, or somatoform disorders.[8]
Although the cause is unknown, psoriasis is believed to have a complex origin that includes genetic pre-disposition, environmental stressors mixed with impaired skin barrier function and impaired immune system.[9] It is an inflammatory immune-mediated disease with autoimmune pathogenic characteristics that affect the skin and other systems. Psoriasis is considered a T-cell-driven systemic disease with massive infiltration of lymphocytes, macrophages and neutrophils in the psoriatic lesions. It is, therefore, clear that the disturbances of the innate and adaptive immune response are responsible for the development and maintenance of psoriatic inflammation.[10]
Psoriasis may coexist with other skin conditions that have clinical overlap, such as atopic and seborrheic dermatitis in the same patient. Diagnostic doubt may arise if the psoriatic lesions are localised to specific sites such as nails, skin folds or the genital area. Histopathology of the skin shows the characteristic pathological features of psoriasis.[11]
Psoriasis cannot be treated as a local condition with outside interventions that only take away the visible symptoms. This study was conducted using constitutional homoeopathic medicines to successfully treat scalp psoriasis, prevent discomfort and improve the patient’s overall quality of life.
MATERIALS AND METHODS
Study design
This was a prospective experimental study.
Sampling
Consecutive sampling.
Sample size
The sample size was 30.
Inclusion criteria
Male and female patients in the age group of 10–70 years, presenting with signs and symptoms of scalp psoriasis that is clinically diagnosed and who are willing to give written informed consent and for those under the age of 18 consent from parents were included in the study.
Exclusion criteria
Scalp diseases such as seborrheic dermatitis and dandruff, pregnant and lactating women and patients with malignancies were excluded from the study.
Diagnostic criteria
The cases were diagnosed by a dermatologist and scoring was done using the Psoriasis Area and Severity Index (PASI) and Dermatology Life Quality Index (DLQI).
Intervention
Individualised homoeopathic medicines selected after repertorisation in suitable doses and potencies.
Methods
The goal of this study was to investigate the efficacy of homoeopathic treatment for scalp psoriasis. The patients who attended the psoriasis research outpatient clinic at the Government Homoeopathic Medical College in Thiruvananthapuram, Kerala, were chosen as study participants. The inclusion criteria were satisfied by 30 patients, who were then chosen. All participants gave their consent in writing after being fully informed. The study was approved by the Institution’s Ethical Committee. With the help of a dermatologist, the patients were clinically identified and case documentation was completed using a standardised case record format specially designed for the purpose.
The gathered data were examined for the PASI score and DLQI following the administration of the homoeopathic medicine. Every 2–3 weeks, the cases were examined.
Homoeopathic principles were used to determine the potency, dose and repetition of the remedy for each instance. Each patient received a single remedy in a potency appropriate to the case’s needs and the minimal required dose. Nothing else was done as long as the patient got well after receiving the dose.
One further dose of the same medication was administered when the patient’s improvement stopped progressing. The next higher strength of the same medicine was administered if it appeared that the prior potency was insufficient to result in a sufficient improvement. Every time it appeared that the totality of symptoms had changed, a fresh examination was conducted and a new medication was chosen. Diet and nutrition plans were recommended in addition to the homoeopathic treatment and the patients were advised to give up smoking, drinking and other addictions. Yoga was advised as a stress-relieving exercise.
Measurement of outcome
The outcome of treatment was assessed based on the improvement in the patient’s symptoms and changes in the PASI score and DLQI before and after treatment.
The PASI includes an assessment of body surface area, erythema, induration and scaling. The severity score ranges from 0 to 72 and is a useful measure to assess response to a particular treatment. The DLQI measures the impact of skin disease on the patient’s quality of life over the past 7 days. It consists of ten items, six dimensions and a summary total score. Each question can be answered with one of four responses: not at all, little, a lot or very much, with scores of 0, 1, 2 and 3, respectively. The total score ranges from 0 (the best score) to 30 (the worst score). It is useful in clinical practice because of its brevity and simplicity.
Plan of analysis
The significance test was used to confirm the final statistical analysis of the study, which was conducted using the relevant statistical techniques. The paired t-test was employed as the DLQI significance test because there were scores before and after therapy. The data, however, were not normally distributed for PASI and hence the Wilcoxon signed-rank test was employed to evaluate significance.
RESULTS
Statistical analysis
As evidenced above [Table 1], the PASI score was not normally distributed and hence the non-parametric equivalent of ‘t’ – the Wilcoxon signed-rank test was applied. The paired ‘t’ test was used for DLQI.
PASI
The median PASI score before treatment was 0.8 (interquartile range 0.37–1.87).
PASI median score after treatment was 0.25 (interquartile range 0.10–0.72).
Out of 30 subjects, 22 had a negative rank with a lesser score for PASI after treatment. None of them scored higher and eight remained the same [Tables 2 and 3].
Inference
The Wilcoxon signed-rank test was performed to determine if there was a statistically significant difference in the mean PASI score before and after treatment. The observed difference was found to be significant on the Wilcoxon signed-rank test (P = 0.001). Therefore, the null hypothesis is rejected and the alternate hypothesis is accepted, that is, there is a significant difference in the PASI score of patients with scalp psoriasis before and after treatment.
Statistical analysis of DLQI
To analyse the pre- and post-treatment changes in the total symptom score, the paired t-test is used. Let X be the total score before treatment and Y be the total score after treatment [Tables 1 and 4].
| Kolmogorov–Smirnova | Shapiro–Wilk | |||||
|---|---|---|---|---|---|---|
| Statistic | df | Sig. | Statistic | df | Sig. | |
| PASI before | 0.217 | 30 | 0.001 | 0.806 | 30 | 0.000 |
| PASI after | 0.252 | 30 | 0.000 | 0.736 | 30 | 0.000 |
| DLQI before | 0.087 | 30 | 0.200* | 0.972 | 30 | 0.600 |
| DLQI after | 0.171 | 30 | 0.025 | 0.893 | 30 | 0.006 |
| PASI after–PASI before | n | Mean rank | Sum of ranks | |
|---|---|---|---|---|
| Negative ranks | 22a | 11.50 | 253.00 | |
| Positive ranks | 0b | 0.00 | 0.00 | |
| Ties | 8c | |||
| Total | 30 |
PASI: Psoriasis area and severity index. aPASI after <PASI before, bPASI after >PASI before, cPASI after=PASI before
| PASI after–PASI before | |
|---|---|
| Z | −4.114b |
| Asymp. sig. (2-tailed) | 0.000 |
PASI: Psoriasis area and severity index, aWilcoxon signed-rank test, bBased on positive ranks
| PASI before | PASI after | DLQI before | DLQI after | |
|---|---|---|---|---|
| n Valid missing | 30 | 30 | 30 | 30 |
| 0 | 0 | 0 | 0 | |
| Mean | 1.1000 | 0.5667 | 9.867 | 3.0333 |
| Median | 0.8000 | 0.2500 | 10.000 | 2.5000 |
| Standard deviation | 1.00781 | 0.68107 | 5.3093 | 2.79758 |
| Percentile | ||||
| 25 | 0.3750 | 0.1000 | 5.000 | 0.7500 |
| 50 | 0.8000 | 0.2500 | 10.000 | 2.5000 |
| 75 | 1.8750 | 0.7250 | 14.250 | 5.0000 |
PASI: Psoriasis area and severity index, DLQI: Dermatology life quality index
Null Hypothesis H0: There is no difference in the DLQI score before and after treatment Alternate Hypothesis H1: There is a significant difference in the DLQI score before and after treatment.
Substituting the values of DLQI
∑d = 205
∑d2 = 2149
n = 30
Paired t formula
Where
SD = 5.08
Paired t = |d|/(SD of d/√n) = 6.83/(5.08/5.47) = 6.83/0.93
t = 7.34
Comparison with the table ‘t’ value
The paired t value at n-1 degree of freedom, that is, 29, at 5% (0.05) level of significance is 2.045, at 1% (0.01) level of significance is 2.756 and at 0.1% (0.001) level of significance is 3.66. Here, the t value obtained is 7.34, which is greater when compared to the t table value at 0.1% level. Hence, we can reject the null hypothesis: H0 There is no difference in the DLQI before and after treatment and can accept the alternative hypothesis, there is a significant difference in DLQI before and after treatment.
Distribution of patients based on PASI score before and after treatment
After administration of individualised Homoeopathic medicines, PASI Score decreased in 22 0ut of 30 cases which shows that homoeopathic medicines are effective in the treatment of Scalp psoriasis [Figure 1].
Distribution of patients based on DLQI score before and after treatment
Following therapy, study participants showed a significant improvement in their Dermatology Life Quality index score [Figure 2].
Improvement of symptoms after treatment
Improvement of patient’s symptoms including erythema, induration and scaling after treatment [Figure 3].
DISCUSSION
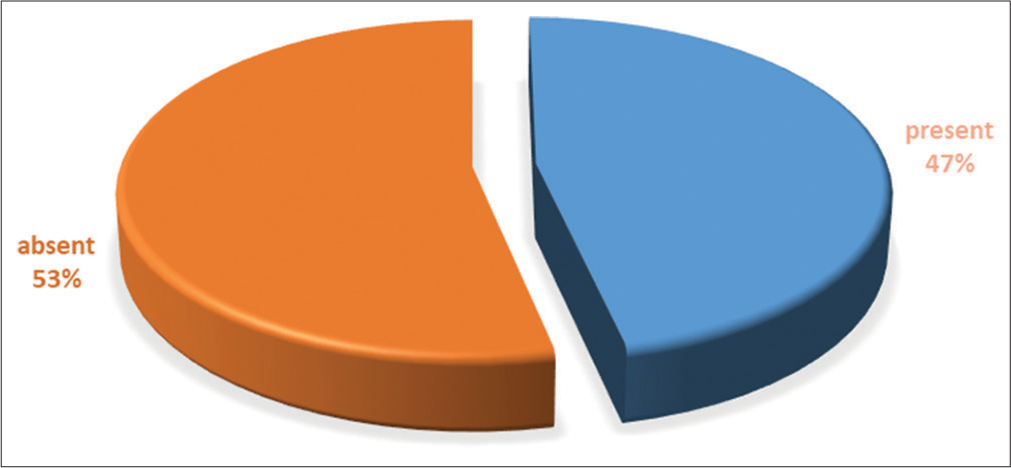
It is clear from the current study of 30 instances that homoeopathy can effectively treat scalp psoriasis. A few findings that came out of the study must be discussed to draw a valid conclusion. Out of the 30 cases included in this study, 22 had significant reductions in erythema, induration and scaling on analysis of the outcomes following treatment, whereas the other eight had no change in these symptoms. According to DLQI evaluations conducted before and after the trial, 28/30 patients’ quality of life improved. Noting changes like psoriasis lesions on the scalp served as the study’s final evaluation. By comparing the PASI and DLQI ratings for the area of psoriasis lesions on the scalp before and after therapy, the study’s overall effectiveness was determined. After the medication was administered, PASI scores decreased in 22 cases whereas remaining unchanged in 8 cases. After receiving treatment, the DLQI ratings dropped in 28 cases and those patients reported an improvement in their quality of life. In the other two cases, there was no improvement in the patient’s standard of living. More than 60% of the patients were male Figure 4 and the age range of 20–50 was the predominant one [Figure 5]. This could be caused by exacerbating variables such as stress, which may be more common in this age range, or by contributory factors such as smoking, alcohol consumption or both.

- Distribution of patients based on psoriasis area and severity index score before and after treatment.
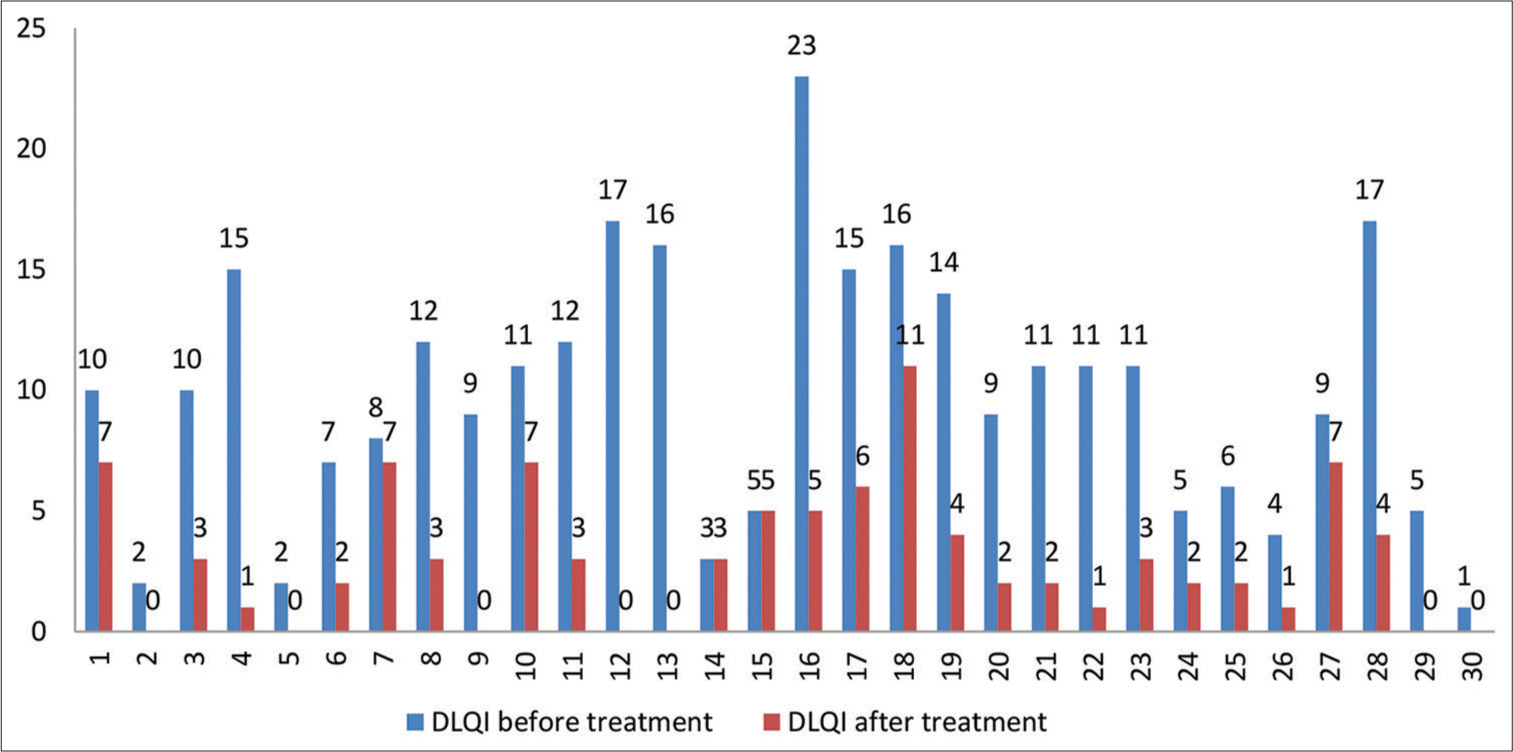
- The dermatology life quality index of patients before and after treatment.
The two habits that were shown to be most significant were smoking and alcohol consumption, which were strongly positively associated in 23.3% of instances. To verify this finding, a thorough investigation with a sizable sample size is needed. Nearly 60% of patients had psoriasis between 1 and 10 years in duration and 40% of cases had it for more than 10 years. A strong positive family history of psoriasis among the first-degree relatives was observed in 46.6% of cases [Figure 6].
This study found that mental stress, including anxiety, food allergies and seasonal exacerbations are the most frequent triggers. In 20% of cases, stress is an important triggering element. Hypertension (two instances), diabetes mellitus (one case), renal calculi (three cases), bronchial asthma (three cases), gastritis, gastric ulcer, irritable bowel syndrome, benign prostatic hypertrophy, migraine and allergic rhinitis are comorbidities that have been observed in these patients [Figure 7]. After the medication was administered, several patients’ signs and symptoms, such as erythema, induration and scaling, were lessened. In ten patients, the signs and symptoms had completely disappeared.

- Distribution of patients according to symptoms before and after treatment.

- Graphical representation of cases according to sex.
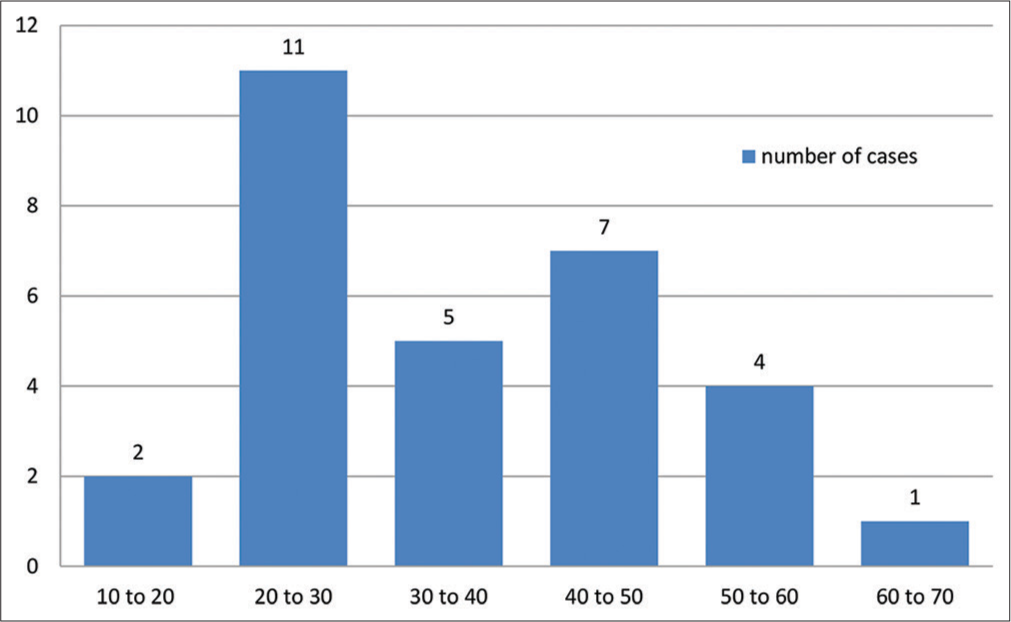
- Patient distribution according to age.
- Distribution of patients according to family history of psoriasis.

- Distribution of patients according to comorbidities.

- Indicated medicine in 30 cases.
In all cases, individually tailored medicines were selected after repertorisation with the Repertorium Homoeopathicum Syntheticum. Sulphur (n=7) in its various potencies was the medication that was prescribed the most frequently in this study. Other medicines which were found more beneficial are Phosphorus (n=4) and Natrum Mur. (n=2) [Figure 8]. In certain instances, nosodes were used as an intercurrent remedy. In some circumstances, the medicine’s potency was increased gradually from 200 to 50 Millesmal potency and wherever necessary the these potencies were repeated. Specifically, erythema, induration and scaling showed improvement in the current study. In some circumstances, improvements could be seen as early as the 1st month, in others, they took 3–4 months, and in still other cases, they took 6 months or more. While some instances did not experience any improvement in induration or scaling during the research period, they did experience improvement in their quality of life and any related complaints, such as itching. Within the research period, the key ways, in which the quality of life has improved, are through better work efficiency, enhanced interpersonal relationships, everyday activities, social and recreational activities and raised confidence levels.
Limitations
The biggest challenge in treating scalp psoriasis was gaining the patient’s trust and persuading them of the seriousness of the illness, the efficacy of homoeopathic treatment, the length of time it might take for the condition to significantly improve and the need to continue the course of treatment. The emotional toll of scalp psoriasis is made worse by the patient’s and their loved one’s anxiety. Although patients anticipate a quick recovery, it takes more time to get such ideal outcomes. Exacerbations and remissions were noted during the study period. It was challenging to determine the precise scores of the disease following treatment. One of the most common mistakes made by patients is waiting too long to diagnose the illness since, for a while, it resembles dandruff. Therefore, almost all of the patients began to use some sort of external dandruff treatment, which not only made the situation worse but also made it last longer.
CONCLUSION
Psoriasis most frequently affects the scalp, which has a detrimental effect on people’s quality of life. Life is let down by the embarrassing and frustrating situations caused by the itch. The most frequent mistake in diagnosis is failing to distinguish the condition from dandruff, which increases the ailment’s length and chronicity. The proper treatment and limiting of impairments depend on early detection and intervention. To investigate the efficacy of homoeopathic similimum in this condition, further long-term research with a bigger sample size and control group that demonstrate the curative and positive benefits of potentised homoeopathic treatment for patients with scalp psoriasis are indicated and required.
Acknowledgments
We would like to express our sincere gratitude to the Kerala University of Health Sciences for the support given to pursue a clinical study on the effectiveness of homoeopathic medicines in the treatment of scalp psoriasis as a topic for the postgraduate thesis, for the research in the field of homoeopathy.
Ethical approval
Ethical clearance of the proposed study was obtained from the Institutional Ethics Committee of Government Homoeopathic Medical College, Trivandrum, Kerala as per IEC No: 2247/C3/2019/GHMCT (1)/01.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Psoriasis in special localizations. Reumatologia. 2018;56:392-8.
- [CrossRef] [PubMed] [Google Scholar]
- Calcipotriol plus betamethasone dipropionate aerosol foam for scalp psoriasis. Clin Cosmet Investig Dermatol. 2019;12:699-705.
- [CrossRef] [PubMed] [Google Scholar]
- Newer trends in the management of psoriasis at difficult to treat locations: Scalp, palmoplantar disease and nails. Indian J Dermatol Venereol Leprol. 2010;76:634-44.
- [CrossRef] [PubMed] [Google Scholar]
- Safety and efficacy of calcipotriene plus betamethasone dipropionate topical suspension in the treatment of extensive scalp psoriasis in adolescents ages 12 to 17 years. Pediatr Dermatol. 2015;32:28-35.
- [CrossRef] [PubMed] [Google Scholar]
- The pathophysiological mechanisms and the quest for biomarkers in psoriasis, a stress-related skin disease. Dis Markers. 2018;2018:5823684.
- [CrossRef] [PubMed] [Google Scholar]
- Current knowledge on psoriasis and autoimmune diseases. Psoriasis (Auckl). 2016;6:7-32.
- [CrossRef] [PubMed] [Google Scholar]
- Current developments in the immunology of psoriasis. Yale J Biol Med. 2020;93:97-110.
- [Google Scholar]
- Topographic differential diagnosis of chronic plaque psoriasis: Challenges and tricks. J Clin Med. 2020;9:3594.
- [CrossRef] [PubMed] [Google Scholar]