Translate this page into:
Understanding the scope of Homoeopathy along with a multidisciplinary integrated approach for holistic management of epilepsy with co-morbidity in children: Case studies
*Corresponding author: Dr. Mrunalika Dhaval Dikshit, Department of Practice of Medicine, Smt. Malini Kishore Sanghvi Homoeopathic Medical College and Hospital, Karjan, Vadodara, Gujarat, India. dr.dikshit16@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dikshit MD, Parikh HM. Understanding the scope of Homoeopathy along with a multidisciplinary integrated approach for holistic management of epilepsy with co-morbidity in children: Case studies. J Intgr Stand Homoeopathy 2023;6:123-32. doi: 10.25259/JISH_62_2022
Abstract
Epilepsy is a complex neurological disorder that affects the patient’s mental and physical development as well as their functioning, especially in children. It also presents with mental and/or physical co-morbidities/disabilities. This manuscript describes the importance of an individualised multidisciplinary integrated approach, including homoeopathy, for the holistic management of epileptic children through two illustrative cases. The team included homoeopaths, paediatricians, paediatric neurologists, physiotherapists, and psychologists in both cases. We aimed to demonstrate the scope of the homoeopathic individualised approach for managing epilepsy and its role in improving the quality of life of patients and caretakers. Both cases involved detailed case-taking, including homoeopathic and clinical perspectives. A multidisciplinary integrated approach enabled a comprehensive clinical diagnosis. An individualised approach was used to form a totality and perform repertorisation to select the most appropriate remedy and potency. Follow-up criteria enabled us to measure the progress. The homoeopathic individualised approach resulted in considerable relief in seizures and a reduction in allopathic medication available only in 1st case. and relief in seizures in both the cases. The functioning of the patient and their quality of life improved considerably in both cases as well. Homoeopathic individualised approach, along with the integrated system, helps in the relief/cure of epileptic episodes, enables a reduction in the use of antiepileptic drugs, and improves associated co-morbidities. Through this approach, holistic care is possible and improves the quality of life of the child and the parents.
Keywords
Epilepsy
Homoeopathy
Individualise holistic approach
Integrated approach
INTRODUCTION
An epileptic seizure is a paroxysmal disorder characterised by abnormal, excessive, and hypersynchronous discharges of neurons leading to alteration of function. Epilepsy is not a disorder but a symptom of underlying brain dysfunction.[1] It is a condition characterised by repeated unprovoked seizures. If seizures are consistently provoked, such as by fever or hypoglycaemia, the term epilepsy should not be used.
The International League against Epilepsy provided a new definition in 2014. Epilepsy is a disease of the brain defined by any of the following conditions:
At least two unprovoked (or reflex) seizures occurring more than 24 hours apart.
One unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk (at least 60%) after two unprovoked seizures occurring over the next ten years.
Diagnosis of epilepsy syndrome.
Epilepsy is considered to be resolved for individuals who had age-dependent epilepsy syndrome but are now past the applicable age or those who have remained seizure-free for the past ten years, with no seizure medicine administered in the past five years.[2]
Classification of the epilepsies
The new multilevel classification of epilepsies is designed to classify epilepsy in different clinical environments [Figure 1]. Where possible, a diagnosis at all three levels should be sought, as well as the aetiology of the individual’s epilepsy.[3]
![Framework for classification of the epilepsies. Denote onset of seizure.[3]](/content/112/2023/6/3/img/JISH-6-123-g001.png)
- Framework for classification of the epilepsies. Denote onset of seizure.[3]
Classification serves many purposes
Provides a framework for understanding the predominant type of seizures in the patient and the other types likely to occur.
Provides potential triggers and prognosis for seizures.
Informs the risks of co-morbidities including learning difficulties, intellectual disability (I.D.), psychiatric features such as autism spectrum disorder, and mortality risk such as sudden unexpected death in epilepsy.
Classification often guides the selection of antiepileptic therapies.[3]
The team of the Institute of Neurology and Neurosurgery focused on the understanding of symptomatic generalised epilepsy. Symptomatic epilepsy is defined as epilepsy after an injury to the brain that is known to be capable of causing epilepsy. Examples are as follows: significant head injury, central nervous system (C.N.S.) infection, stroke, brain tumour, and surgery. There is commonly more than one seizure type in symptomatic generalised epilepsy. The seizures are commonly resistant to medication, and often multiple medications are required. These epilepsies have a higher comorbid I.D., cerebral palsy, or other developmental problems.[4]
Neonatal seizures
Neonatal seizures are fairly common. They are defined as the occurrence of sudden, paroxysmal, and abnormal alteration of electrographic activity at any point from birth to the end of the neonatal period. When a patient with neonatal seizures is encountered, it may be the first clinical sign of a serious neurologic disorder. Thus, rapid recognition and evaluation are required to identify and treat the underlying aetiology, prevent further brain injury and extinguish the seizure activity. At birth, the brain is in a state of continued development; some areas are immature. If the neonatal brain is pathologically provoked, it may cause seizures. Due to its immature state, the neonatal brain is prone to seizures due to an imbalance between neuronal excitation and inhibition. The factors causing this imbalance include metabolic disturbances, hypoxic conditions, an inborn error of metabolism, intracranial haemorrhage, C.N.S. infection, thromboembolic, neonatal epilepsy syndrome and congenital brain malformation. The prognosis of neonatal seizures depends on the underlying aetiology. If the electroencephalogram (E.E.G.) is normal, the prognosis is excellent; conversely, an abnormal E.E.G. may indicate a poor prognosis and the development of conditions such as cerebral palsy and epilepsy. The presence of spikes in E.E.G. indicates a 30% risk of developing future epilepsy. The mortality rate of neonatal seizures is reported to be as high as 20%. In survivors, neurologic impairment, disability, developmental delay, and epilepsy are common. Both the cases studied in this paper demanded a complete understanding of the evolution of neonatal seizures at the time of neonatal age.[5]
Epilepsy with co-morbidities
Many epilepsies are associated with co-morbidities such as learning, psychological and behavioural problems, or psychosocial concerns ([Figure 1], left vertical oval). In the more severe epilepsies, a complex range of co-morbidities may be seen, including motor deficits such as cerebral palsy or movement disorders. The presence of co-morbidities is considered for every patient with epilepsy at each stage of classification, enabling early identification, diagnosis, and appropriate management.[3]
Epilepsy and homoeopathy
According to Dr. Hahnemann›s disease classification, epilepsy is a chronic miasmatic periodic disease. There are more than 500 remedies in homoeopathy for seizures with a specific indication for episode/type of seizures. As epilepsy is a chronic disease, it requires a constitutional or deep-acting remedy. Not all the above-mentioned remedies can be classified as constitutional. However, a specific remedy may help control an acute seizure.
Several papers are available that provide a focused, detailed clinical perspective as well as a deep understanding of homoeopathic disease classification and therapeutic approach. All have concluded that homoeopathy helps in the management of epilepsy through an individualised approach.[6-10] However, all these papers are based on materia medica and therapeutics; none have examples of cases.
Therefore, we present two case studies focusing on the outcome of cases of epilepsy in children through a homoeopathic individualised integrated approach.
CASE SERIES
Case 1
Baby C.V.S (case No 9165), 3.5 years (D.O.B – 28/8/2013), was brought by parents on 20.1.2017. The parents reported seizures, delayed speech, and non-cooperative behaviour.
Chief complaints
She is suffering from epilepsy, poor fine motor function , non- cooperative and non communicative behaviour and yet speech is not developed [Table 1].
| S. No. | Location | Sensation | Modality | Accompaniment |
|---|---|---|---|---|
| 1. | C.N.S. | Birth/H: Breech presentation, full term, LSCS, cried immediately after birth, Weight: 2 kg. | ||
| Onset: 3rd day of life | H/O refused to suck/eat | A/F-hypoglycaemia | ||
| D: 13 days | H/O seizures, | Rx.-Inj. cefixime | ||
| Diagnosed with hypoglycaemic seizures | Inj. genta | |||
| Tonic posturing (from documents) | Inj. Ca Gluconate, 25 cc+D25% | |||
| RBS-32 | Inj. Phenobarbital | |||
| Hospitalisation | Inj. Phenytoin | |||
| After discharge/ | Ictal symptoms: Frothing from the mouth, up | > AEDs (details not available) | ||
| frequency-7-8 times/day | rolling of eyeballs, sudden | |||
| duration-2-3 min. | blankness | |||
| At 6 months of age | Headholding not developed | >Physiotherapy | ||
| (1) From 2013 till today | Ictal symptoms: - GTCSs | valparin 5 mL/BD (2015) | ||
| Mouth | frothing | <ANGER3 | ||
| Eyes | up and rolling | |||
| F-Once/7-15 days | Loss of awareness | |||
| D-1-2 min | ||||
| (2) From 2015 till today | Stretching 3 | |||
| Fingers both hands | No loss of awareness | |||
| F: 8-9 times/day D: 1 min. | ||||
| At 3.5 years of age | Gross motor functions developed in a timely manner. Fine motor skills not developed (eating, writing) |
> After physiotherapy - 3 | ||
| Mind | Non-cooperative Poor eye contact - 2 Understanding poor - 2 SOCIALISATION poor - 2 | |||
AED: Antiepileptic drug
Associated complaints [Table 2]
Mo. Obstetric/H: G3P2A1, G1: Male 12 years old (Normal), G2: Natural abortion, G3: Patient MO. Antenatal/H: PIH, (AHT Rx).
| S. No. | Location | Sensation | Modality | Accompaniment |
|---|---|---|---|---|
| 1. | R.S. | Nasal discharges - 2 | A/F Change of weather | |
| Since birth | Sneezing - 2 | > Allopathic Rx | ||
| F-related to modality | Fever - 2 | |||
| D: 4-5 days | ||||
| 2. | General | HT-87.5 CM, Wt.-10.3 kg, H.C-43 cm | ||
| Diet eats in excessive quantity3 |
Marital history of parents: non-consanguineous.
Stool: Hard 3. Since last month, 3–4 times/day. Semisolid, yellowish, no abdominal pain.
Craving: Sweets 3.
Examination
H.T.: 87.5 cm WT.: 10.3 kg H . C : 4 3 c m
P/A: SOFT RS/CVS/CNS: N.A.D.
Investigation
9/5/2015, BERA: Normal hearing
8/8/2015: E.E.G. Bioccipital, interictal epileptic form discharges suggestive of focal epilepsy
Magnetic resonance imaging (M.R.I.): Not available
30/11/16: Ophthalmic opinion: Bil eye -> Visual error reflex (near vision). Advised glasses, but the patient refused.
Diagnosis
Focal epilepsy + G.D.D. + recurrent simple rhinitis + speech not developed + visual error reflex + malnutrition (grade II) + moderate I.D. with mild autism (psychologist assessment advised).
Patient as a person
Her father is a health worker at P.H.C. The parents’ nature is fairly calm, but the mother is anxious about her daughter’s complaints and behaviour. She is obstinate – 3, demanding – 3, moody – 3, and aversion to touch – 3. She is irritable – 3 –cranky – 3, throws things – 3 and beats – 3 and leads convulsions 3. She cries – 2 and shouts – 2 without any reason. She obstinately – 3 demands things but rejects them when they are offered. If anyone tries to console her, she becomes crankier. She likes dancing – 2 and has a fear of being alone – 2.
Approach
Kent: Characteristics, qualified mental symptoms, and characteristic physical general and particular symptoms.
Totality
Repertorial syndrome [Figure 2]
Consolation < anger – 2
Shouting without reason – 2
Cry without reason – 2
Beating others without reason – 2
Fear of being alone – 2
Like dancing – 2
Obstinacy – 3
Cranky – 3
Moody – 3
Wants more food
C.R. Sweet – 3
Hard stool – 3
Coryza – from change of weather
Sneezing – from change of weather
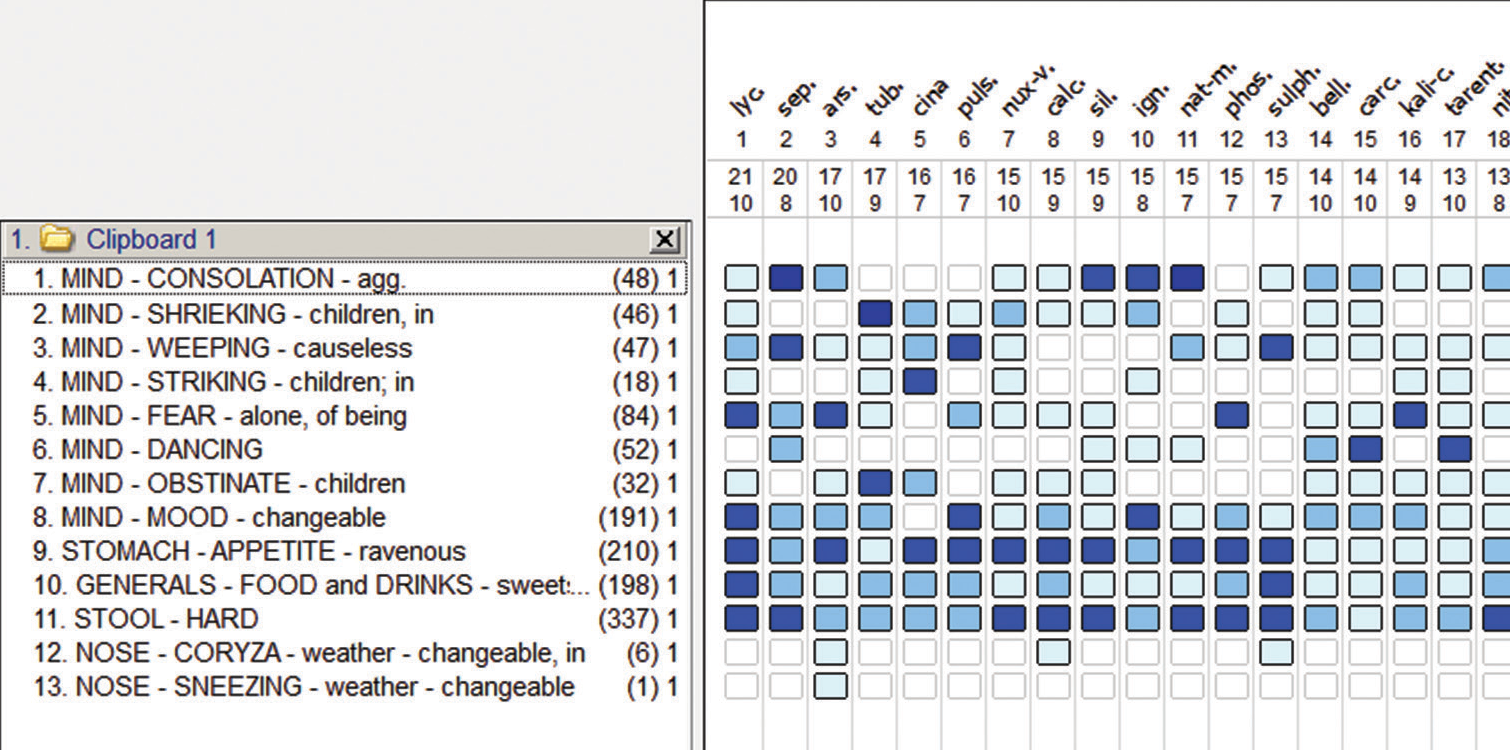
- Case 1-Reptorisation sheet.
Thermal differential field
Chilly remedies: Sepia,Cina, Calc.Carb, Silicea, Igantia, Phos, Tarentula.
Hot-Chilly remedies: Lyco., Nat.Mur, Carcinosin
Hot remedies: Tuberculinum, Sulphur
Potential differential field [Table 3]
➜ Closely coming remedies: Cina, calc carb, and tarentula.
➜ Considering touchiness, crankiness, convulsion modality, and thermal state, cina was selected.
| Name of remedy | Sepia | Cina | Calc carb | Silicea | Ignatia | Phosphorus | Tarentula |
|---|---|---|---|---|---|---|---|
| Anger -*→ Convulsion | - | 1 | 3 | - | - | - | - |
| <Touch 3 | - | 2 | 1 | 2 | - | - | 3 |
| Striking from anger 3 | - | - | - | - | - | - | - |
| Reject the things when offered 3 | - | 2 | - | - | - | - | - |
| 5/3 | 4/2 | 2/1 | 3/1 |
Susceptibility: Moderate
Sensitivity: Moderate to high
Dominant miasm (DM): Tubercular
Reason: Sudden onset, fast progress, structural, irreversible, and static pathology in the brain with excessive electrical brain discharge. Post hypoglycaemic seizures ➜ Possibility of neonatal hypoglycaemic brain injury.
Treatment: Cina 200 1P/Weekly (W)
Advice: Physiotherapy and psychologist consultation, continue antiepileptic drug (AED), E.E.G., and M.R.I.
Follow-up criteria
Follow ups-[Table 4],
| Date/Duration | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 20/1/2017 to 14/4/2017 (4 months) | ||||||||||||||||||||||||||||||||
| A | > | o > | > | > | > | > | S | S | Bisyllabic | > | ||||||||||||||||||||||
| B | > | o 30/3/2017. | S.Q | S.Q | >/once/ month |
96 | 40 | 4/4/2017 Normal |
1/month | -- | ||||||||||||||||||||||
| Stool c/o: Within one month-0, Seizures-once/week: Stretching in fingers. | ||||||||||||||||||||||||||||||||
| 14/4/2017-Ht.-87.5 cm, Wt.-10.6 kg, HC-43.5 cm Last episode 30/3/2017: single episode, 15 min: Generalised seizure. Follow command: Daily activity, bring water, Food intake: quantity reduced. 21/2/2017: Psychologist’s opinion, moderate I.D. (IQ-40) with mild autism (Autism score/AS-96) (play and behaviour therapy and modification, speech therapy, home-based management-report attached). R.S.- >3 with puls 200 TDS/3 days. Till 14/4/2017: CINA 200 1P/Weekly (W), On 14/4/2017: CINA 200 1P/W+TUB 1M 1P Intervention of I.R.: Seizure episode → Intervention with Tuberculinum |
||||||||||||||||||||||||||||||||
| 12/5/2017 to 22/3/2019 (2 years and 2 months) | ||||||||||||||||||||||||||||||||
| A | >2 | >2 | >2 | >2 | >2 | All | Achieved (A) |
A | small sentences | >2 | ||||||||||||||||||||||
| B | >2 | 30/3/2017 | > | ½-0>3 | >3 | Dec. 18 →94 | Dec. 18→48 | -- | Once/month | |||||||||||||||||||||||
| 22/3/2019-Ht.-110 cm, Wt.-13 kg, HC-44 cm Seizures: only while angry, stretching in fingers intensity>2. AED: May 17 OD, From August 18: stopped as advised by the paediatrician. Cognitive development: normal schooling started, no complaints from school. R.S.: 4 Episode>3 with A.R. • Cina 200 1P/HS/W ^ 3P/ March 19: Cina 1M 3P/W |
||||||||||||||||||||||||||||||||
| 21/5/2019 to 25/12/2020 (3 years) | ||||||||||||||||||||||||||||||||
| A | 0 | 0 | >3 | N | >3 | N | A | 2/lost control |
N | N | ||||||||||||||||||||||
| B | 0 | 0 | 0 | 0 | 2>3 itself | -- | -- | -- | No session | + | ||||||||||||||||||||||
| 10/7/2020-Ht.-113 cm, Wt.-15 kg, HC-45 cm From 1/12/2020-Trembling in hand2-occasionally (not other history/symptoms available). Psychological assessments were not done. As the family had moved elsewhere, the medicine was sent via courier. Parents: Happy and satisfied with the child’s progress. • Cina 1M/3P/W • Tuberculinum 1M 1P/One dose |
||||||||||||||||||||||||||||||||
| 27/4/21 to 26/11/22 (5 years) | ||||||||||||||||||||||||||||||||
| A | 0 | 0 | 0 | N | N | N | A | A | N | N | ||||||||||||||||||||||
| B | 0 | 0 | 0 | 0 | 0 | 0 | 55 | 50 | Stopped | >3 | ||||||||||||||||||||||
| 26/11/22 - Ht.-126 cm, Wt.-20 kg, HC- 45 cm Trembling in hand-0 (within one month), attends school without problems, identifies all things, difficulty in writing. Psychologist’s opinion: 26/11/22, I.Q. 50, moderate I.D., AS: 55 (<70: Indicates no autism) (report attached) → Parents want to continue treatment for better scholastic performance. • Cina 1M/3P/W |
||||||||||||||||||||||||||||||||
AED: Antiepileptic drug, IQ: Intelligence quotient, OD: Once daily
Follow-up evaluation
➔ Child becomes calm and achieves bladder and bowel control.
➔ Acute episode of respiratory infection initially handled with acute remedy and later with deep-acting remedy.
➔ Behavioural improvement continued despite fewer psychotherapy sessions.
➔ Normal schooling started, indicating improvement in cognitive function.
➔ Similimum helps to stabilise susceptibility, leading to stoppage of seizures and reduction in AEDs.
➔ Moderate ID (40) with mild autism (AS-96): End of 5 years IQ-48 and AS is 55, indicating moderate I.D. with no autism.
➔ Tuberculinum helped to stop the episodes of seizures, and R.S. c/o.
Learning
Detailed birth history and evolution of disease help to derive the current clinical state.
Qualified mental symptoms and observation help in the selection of similimum.
Moderate susceptibility with high sensitivity requires moderate potency.
Tuberculinum as an intercurrent definitely helps to stabilise the susceptibility and hasten the process of recovery.
Withdrawal of AEDs in such cases is challenging; however, with the integrated approach and regular intervention of homoeopathy, it is possible.
Changes in E.E.G. findings, improvement in the I.Q., and achieving bladder and bowel control are proof of the process of recovery. The individualised remedy, along with the interdisciplinary approach, plays a role in holistic improvement.
Case 2
Parents brought their 11-year-old son (D.O.B- 30/9/2008) (case no. 12039) in a bedridden state on 15.11.2019 with frequent episodes of seizure since birth. They had tried several AEDs and followed the keto diet without a satisfactory outcome. Parents are frustrated from frequently changing epileptic drugs and doses.
Current clinical state [Table 5]
| S. No. | Location | Sensation | Modality Accompaniment |
|---|---|---|---|
| 1. | C.N.S. Birth |
Birth/H: FTND, BCIAB, Weight-2.8 kg | |
| O: 3rd day of life | Generalised clonic seizures, Up rolling eyeballs, | A/F- hypoglycaemia>+AEDs | |
| F-7-8 times/day D-15-20 min | frothing | ||
| F-20-25 time/day 7-8 jerks at a time | Quick, generalised, involuntary jerks | ||
| 5th day | Hypoglycaemic seizure with Jaundice | ||
| At present | Pre-ictal: Shrieking3 | (Since last year) Syp. | |
| F-0-4 time/day, D-5-15 | Ictal symptoms: -generalised clonic seizures, | Divalproex 300 mg/BD, | |
| Min. | Up rolling | Tab. lamotrigine 25 DT/BD, | |
| Eye | frothing | Tab perampanel 2 mg/2 tab/ | |
| Mouth | OD, Syp. Levo-carnitine 5 mL/OD | ||
| F-15-20 time/day 7-8 at a time | Same | ||
| General development | Head holding, sitting, standing, speech not achieved Generalised spasticity3, Drooling3 Hearing normal Social development not achieved |
Not>even with physiotherapy | |
| Mind | No understanding about family members, strangers, place, things. Psychologist’s opinion: profound I.D. (IQ-5) |
AED: Antiepileptic drug
MO. Obstetric/H: G2P2A0, G1: Patient, G2: 2 ½ years male: Normal
Mother antenatal/H: NIL
Parents’ marital history: Non consanguineous
Family/History: paternal grandparents: Hypertension, paternal uncle: died four years prior due to oral cancer
O/E: Wt: -21 kg HT-125 cm P-94/min, R S /
CVS/P/A-NAD
C.N.S.: Tone: Hypertonia +3 in all Limbs Power: Bil. UL/LL+
Diagnosis: quadriplegic spastic cerebral palsy + symptomatic generalised epilepsy + profound I.D.
Investigation [Table 6]
| 9/2/10 | E.E.G. | Abnormal sleep E.E.G. showing generalisation and multifocal Bilateral Mainly post-epileptic form abnormally with dysfunction |
| 16/2/10 | M.R.I. | The bilateral frontal periventricular white matter with associated volume |
| loss suggestive gliosis sequel of hypoxic-ischaemic brain damage. Corpus callosum and subcortical cerebral atrophy | ||
| 17/1/14 | E.E.G. | Epileptic form activity of myoclonic in nature from the left occipital hemisphere with secondary generalisation with diffuse slowing from the left anterior hemisphere. |
E.E.G.: Electroencephalogram, M.R.I.: Magnetic resonance imaging
Patient as a person
Parents are educated and oriented. They brought him with the hope of reducing the frequency of seizures. They are aware of the prognosis of the disease condition.
He looks fair, lean, and thin, remains in his own world, prefers to play alone, and becomes angry when any guest comes home or brings him outside. He is fastidious – 2, has an aversion to touch – 3, and startles – 3 from noise.
Observation: Continuous nodding of head - 3
Non-repertorial approach: Eliminating symptoms:
Selection of remedy: Nat mur
Susceptibility: Low
Sensitivity: Moderate
Fundamental miasm: Psora + Syphilis
D.M.: Tubercular ➜ Syphilis
Reason: Sudden onset, fast progress, Structural, irreversible, static hypoxic ischaemic pathology leads to atrophy of brain structure and brain malformation with excessive electrical brain discharge.
Treatment started: Nat mur 0/1 3P/W
Advice: Admission for physiotherapy and psychotherapy, continue AEDs
Follow-up criteria:
Follow up Details: [Table 7]
| Date/Duration | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Nov. 19 to July 20 (9 months) |
||||||||||
| A | > | S | > | 5 min | > | >/7–8/day (4–5) | >2 | S | S | S |
| B | S | S | S | S | S | S | Admitted/weekly/month | S | -- | -- |
| Started responding to sounds of a known person/physician | ||||||||||
| • Nat mur 0/1 3P/W ➜ N. M 0/2 daily HS | ||||||||||
| July 20 to Nov 21 (2 years) |
||||||||||
| A | >2 | >2 Once/15 days | >2 | 5 min | s | >2/3–4/day (2–3) | >2 | babbling | >2 | > |
| B | > | S | > | > | > | > | same | SQ | -- | -- |
| Started head holding, O/E: Tone: > + Hypertonia, Power: SQ | ||||||||||
| • Tuberculinum 0/4 1P H.S. alternate week to W • Nat mur 0/2 HS daily ➜ B.D. |
||||||||||
| Nov 21 to July 22 (2 years and 8 months) |
||||||||||
| A | >2 | >2 once/2–3 month | >2 | 5 s | 0 | >3,3-4/day, (1–2) | >3 | monosyllabic | >2 | >2 |
| B | > | > | > | > | > | > | 1/month | S.Q. | Done > | 7 |
| Aware of his name E.E.G.: Nov 21 Abnormal, slow spike and wave complex, s/o: Symptomatic generalised epilepsy Major supported: sitting 10 min., standing 5 min. |
||||||||||
| • Tuberculinum 0/4 1P HS/W • Nat mur 0/2 BD daily |
||||||||||
E.E.G.: Electroencephalogram
Follow-up evaluation
➔ Considering pathology and multiple types of seizures, susceptibility and sensitivity demanded a frequent repetition of deep-acting remedies and frequent anti-miasmatic remedies in 50 millesimal potencies.
➔ After two years, the child started sitting and standing with support. The state and stage of pathology demanded daily rehabilitation, but after a few months, only one therapy session per month was possible. Due to this, there was limited improvement developed in gross motor, fine motor, and cognitive function.
➔ Deep-acting remedy with an intercurrent remedy in frequent repetition helps to control seizures without modification of AEDs, which had previously been frequently modified.
➔ With the help of similimum, susceptibility stabilised002C and a gradual reduction in seizure episodes occurred, with improvement in the patient’s physical capacity.
Learning
Multiple types of seizure presentations require skill to understand the clinical state, all of which help in case taking.
The concept of eliminating symptoms and observation helped in the selection of similimum.
Low susceptibility with moderate sensitivity required 50 millesimal potency with frequent repetition.
The case demanded regular stimulation of susceptibility with intercurrent remedy It hastened the process of recovery.
DISCUSSION
Both cases have different types of seizures, pathology, and associated psychological and neurological co-morbidities, which demand skills for case taking, recording, and understanding of clinical stage, prognosis, and management strategy even with limited data/investigation of previous history in rural set-up. Both cases focus on the importance of the repertorial and non-repertorial approaches, eliminating symptoms/observation for the selection of deep-acting individualised remedies with the demand of an integrated approach. Case 1 demanded a centesimal scale in moderate potency with infrequent to frequent repetition and I.R. in infrequent repetition, while Case 2 required 50 millesimal potency with frequent repetition and I.R. also in frequent repetition. It reflects the understanding of assessments of susceptibility, the need for different scales, and the role of I.R. in epilepsy management. The presentation of epilepsy with co-morbidities in cases reflects the state and stage of pathology. That understanding helps to plan the therapeutic problem definition and resolution. Its impact on deciding the possibility to tapper/withdraw/continuation of AEDs in epilepsy management and also assess the scope and limitation of homoeopathy. In Case 1, child-free from seizures and AED, and improvement is possible in cognitive and autistic behaviour, while in Case 2, reduction of seizures without modification in AEDs and improvement is possible in cognitive as well gross motor function. It reflects homeopathy helps to stabilise the susceptibility so it leads to a reduction of seizures, withdrawal/stabilise doses of AEDs, and improved functional capacity. In Case 1, improvement in co-morbidity is possible with minimal therapy sessions, while Case 2 demanded frequent therapy sessions. That reflects the understanding of the clinical state and stage of diseases. Through this approach, holistic care is possible and improves the quality of life of the child and the parents as well.
CONCLUSION
The cases reflect the concept of a homoeopathic individualised and integrated approach that helps in the holistic management of epilepsy in children with/without co-morbidities. The cases reflect the importance of case-taking, observation, and understanding of various types of epilepsy, which helps in the understanding of comprehensive diagnosis for management. That focuses on the importance of the knowledge of physicians [Aphorism 3]. The concept of assessment of susceptibility and sensitivity helps in the selection of scale and posology. Moreover, focusing on the sizing of the case helps in the selection of the most similar remedy as well as potency with repetition at an appropriate time. The therapeutic problem definition and therapeutic problem resolution’s assessments, helps in formulating follow-up criteria in such cases. The study of follow-ups reflects the importance of remedy response evaluation and understanding the role of deep-acting as well as intercurrent remedy. I.R. hastens the action of deep-acting remedies and facilitates the process of recovery. Homoeopathy helps control the need for AEDs and the discontinuation of AEDs in cases of epilepsy with the integration of specialists. Homoeopathy and rehabilitation play a crucial role in improving the child’s functioning capacity and modifying the quality of life of the child as well as the parents. Through the cases, understand the scope and limitations of homoeopathy in the management of epilepsy with/without co-morbidities in children.
Acknowledgment
The authors would like to thank Dr. Dilip Nandha for guidance in the preparation of documents.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient consent not required as patient identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (A.I.)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (A.I.)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using A.I.
Financial support and sponsorship
Nil.
References
- Approach to the child with epilepsy In: Pediatric epilepsy. Ch. 1. Europe: McGraw-Hill Education Publishers; 2012. p. :1.
- [Google Scholar]
- ILAE official report: A practical clinical definition of epilepsy. Epilepsia. 2014;55:475-82.
- [CrossRef] [PubMed] [Google Scholar]
- ILAE classification of the epilepsies: Position paper of the ILAE commission for classification and terminology. Epilepsia. 2017;58:512-21.
- [CrossRef] [PubMed] [Google Scholar]
- Symptomatic generalized epilepsy, institute of neurology and neurosurgery, at Saint Barnabas. Available from: https://www.inst-neuro.com/services/epilepsy/symptomatic-generalized-epilepsy [Last accessed on 2023 Oct 31]
- [Google Scholar]
- Neonatal seizure: National Library of Medicine. 2023. St. Petersburg: Star Pearls Publishing; Available from: https://www.ncbi.nlm.nih.gov/books/NBK554535/#__NBK554535_ai__[Last accessed on 2023 Oct 31]
- [Google Scholar]
- An overview of epilepsy with a note on homoeopathic approach. Int J Homoeopath Sci. 2021;5:224-9.
- [CrossRef] [Google Scholar]
- Homoeopathic approach to epilepsy. 2022. Available from: https://thedailyguardian.com/homeopathic-approach-to-epilepsy [Last accessed on 2023 Oct 31]
- [Google Scholar]
- Homoeopathic treatment of primary-idiopathic seizure. 2017. Innovative Veterinary. Available from: https://ivcjournal.com/homeopathic-treatment-seizures [Last accessed on 2023 Oct 31]
- [Google Scholar]
- Epilepsy-homoeopathic treatment and homoeopathic remedies. 2019. Myupchar. Available from: https://www.myupchar.com/en/doctors/mumbai/malad-east/homeopathy/dr-rachita-narsaria-9447 [Last accessed on 2023 Oct 31]
- [Google Scholar]
- Homoeopathy for epilepsy treatment. 2011. Homoeopathy for everyone. Available from: https://hpathy.com/author/manish77 [Last accessed on 2023 Oct 31]
- [Google Scholar]