Translate this page into:
The efficacy of Hamamelis 30 in the management of varicose veins and its complications using revised venous clinical severity score tool and peripheral venous Doppler study
*Corresponding author: Dr. Blany John Lobo, MD, Department of Homeopathic Pharmacy, Fr Muller Homoeopathic Medical College, Deralakatte, Karnataka, India. blanyjohnlobo@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Lobo BJ. The efficacy of Hamamelis 30 in the management of varicose veins and its complications using revised venous clinical severity score tool and peripheral venous Doppler study. J Intgr Stand Homoeopathy 2021;4(2):49-54.
Abstract
Objectives:
The homoeopathic remedy, Hamamelis, has been extensively used to treat varicose veins. However, scientific research conclusively proving its utility is lacking. This study was performed to ascertain the remedy’s therapeutic utility and efficacy in treating varicose veins and its complications using the revised venous clinical severity score (VCSS) tool and Doppler studies.
Materials and Methods:
A prospective uncontrolled experimental study with purposive sampling was performed; the subjects were selected from the outpatient department. A total of 32 cases, fulfilling the inclusion and exclusion criteria were clinically examined. The VCSS and Doppler test before and after treatment with Hamamelis 30 were performed.
Results:
The Wilcoxon signed-rank test was applied and the change in the median VCSS was found to be statistically significant. P-value of the pre score was 5.53 ± 4.15 and that of the post score was 3.45 ± 2.36 with a mean change of 2.09 ± 2.87 and 37.69% improvement with P-value of 0.000 < 0.01. The Doppler study showed no significant change or improvement.
Conclusion:
This study revealed that the homoeopathic remedy Hamamelis 30 is effective in the management of varicose veins and its complications by ameliorating symptoms and improving the VCSS. However, the Doppler study reports showed no changes or improvement perhaps due to the short period of treatment.
Keywords
Hamamelis
Venous clinical severity score
Venous Doppler
INTRODUCTION
Varicose veins are defined as dilated, tortuous, subcutaneous veins 3 mm in diameter when measured in the upright position with demonstrable reflux. They are a common global health problem found in all ages and both sexes. The prevalence is known to increase with age and due to standing/walking <4 h/day and excessive lifting.[1] Although patients may be asymptomatic, aching pain, discomfort, pruritus, and muscle cramps frequently occur. Complications such as edema, eczema, lipodermatosclerosis, ulceration, phlebitis, and bleeding are common. The basic element in the treatment of chronic venous disease is compression therapy.[2] The cost of investigations and treatment is very high. In the Indian scenario, varicose veins are very common among the lower socio-economic class and the condition can even compel people to change their occupation.[3] Hamamelis virginiana, taken internally or externally, is a popular remedy for treating varicose veins, phlebitis, and inflamed veins.[4] The leaves and bark of the North American witch hazel H. virginiana may be used to produce an astringent, also referred to as witch hazel, and is used medicinally.[5] Hamamelis has been known to improve microcirculation, capillary flow, vascular tone, and to strengthen the connective tissue of the perivascular amorphous substrate and avoid the complications of varicose veins.[6] The striking features of this remedy are venous congestion, bleeding, distension of veins, and soreness and dark blue purple appearance of the skin, especially of the lower limbs with ulcers that bleed black blood.[7]
A venous Doppler ultrasound is a diagnostic test used to check the circulation in the large veins of the extremities leg or arms and shows the blockage in the veins by a blood clot or “thrombus” formation. The revised venous clinical severity score (VCSS) is the American Venous Forum’s modification of the clinical score of the Clinical, Etiologic, Anatomic, and Pathophysiologic (CEAP) classification of chronic venous disease. It was designed to be a quantifiable measure of disease severity and is sufficiently dynamic to measure change in response to treatment. The revised VCSS coupled with the clinical CEAP classification provides a standard clinical language to report and compare differing approaches to cardiovascular disease management.[8] The 2-year recurrence rate of varicose veins after radiofrequency treatment is 14%; after vein stripping, it is 21%. Moreover, no treatment can prevent the occurrence of new lesions.[9]
Hamamelis, when used as a specific remedy for varicose veins, has a record of producing results in a cost-effective manner, without having to resort to surgery. In a developing country like India, where patients cannot afford surgery, homoeopathic medicines are simple, safe, and cost effective. This study aimed to establish the therapeutic utility and efficacy of Hamamelis in the 30th centesimal potency (30C) in the management of varicose veins and their complications. Considering the above limitations of the conventional system, the present study focused on evidence-based observations, using the validated VCSS tool and peripheral venous Doppler to understand the role of homoeopathy in varicose veins.
MATERIALS AND METHODS
This was a prospective experimental case study with no control group taken to prevent ethical pitfalls regarding patients not on any treatment. The subjects for the study were selected using purposive sampling, from the patients who reported to the Outpatient Department of Father Muller Homoeopathic Medical College and Hospital, Deralakatte, Karnataka. A total of 60 subjects who fulfilled the inclusion criteria were initially enrolled for the study for 2 years.
Inclusion criteria
The following criteria were included in the study:
Subjects aged between 20 and 80 years
Patients diagnosed with varicose veins
Patients presenting with complications of varicose veins
Patients of both sexes.
Exclusion criteria
The following criteria were excluded from the study:
Terminally ill patients
Patients who require life support.
All patients were informed about the study and its procedures; written consent was obtained from each patient. Their cases were defined using a Standardized Case Record with VCSS score forms charts attached. Finally, 32 patients completed the study and comprised the sample. All the patients were screened for varicose veins and the related complications ulcer, bleeding, lipodermatosclerosis, edema, skin pigmentation, eczema, cellulitis, and assessed using the VCSS tool. The revised VCSS tool is designed to qualify and quantify the classification of chronic venous disease clinically into ten different categories; it is sufficiently dynamic to measure even minor changes in response to treatment. The subjects included in the screening were sent for peripheral venous Doppler study before and after treatment for one or both lower limbs as required. Hamamelis 30C was used since it is a standard potency used in practice in general and at our institute. It is also a middle potency and was used here because in pathological conditions, we cannot use higher potencies and very low potencies since they will either not act or cause severe aggravation. Hamamelis 30C was administered orally twice a day for 2 months to all the patients half an hour before food. The patients were followed up every 2 weeks or month as per their convenience. The frequency of twice daily was used considering the principles of homoeopathic posology as well as the state and stage of disease, susceptibility of patient, and symptom similarity.
The collected data were analyzed and summarized using frequency, percentage, and mean and standard deviation. The significance was assessed using the Wilcoxon signed-rank test and Chi-square test. To determine the changes in the Doppler outcomes and VCSS, the Chi-square test was used.
RESULTS
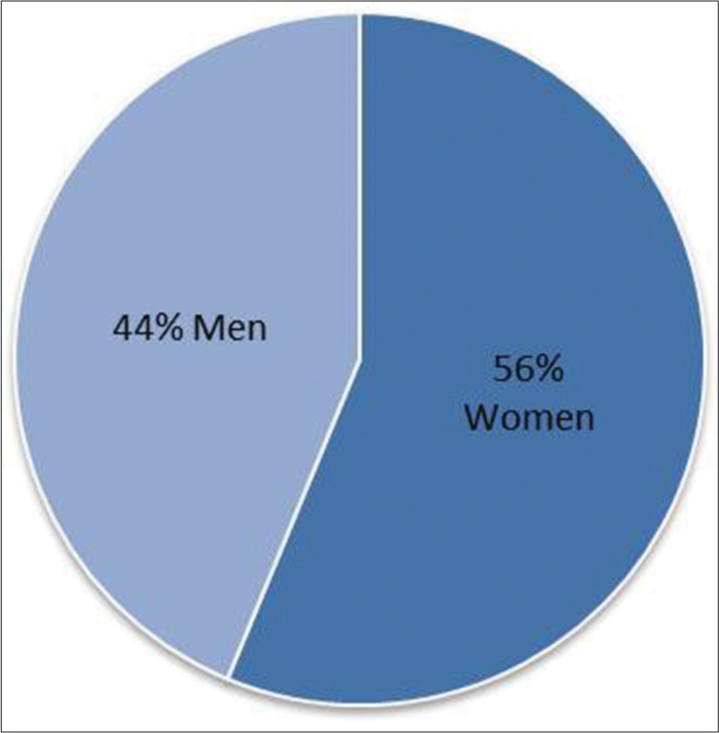
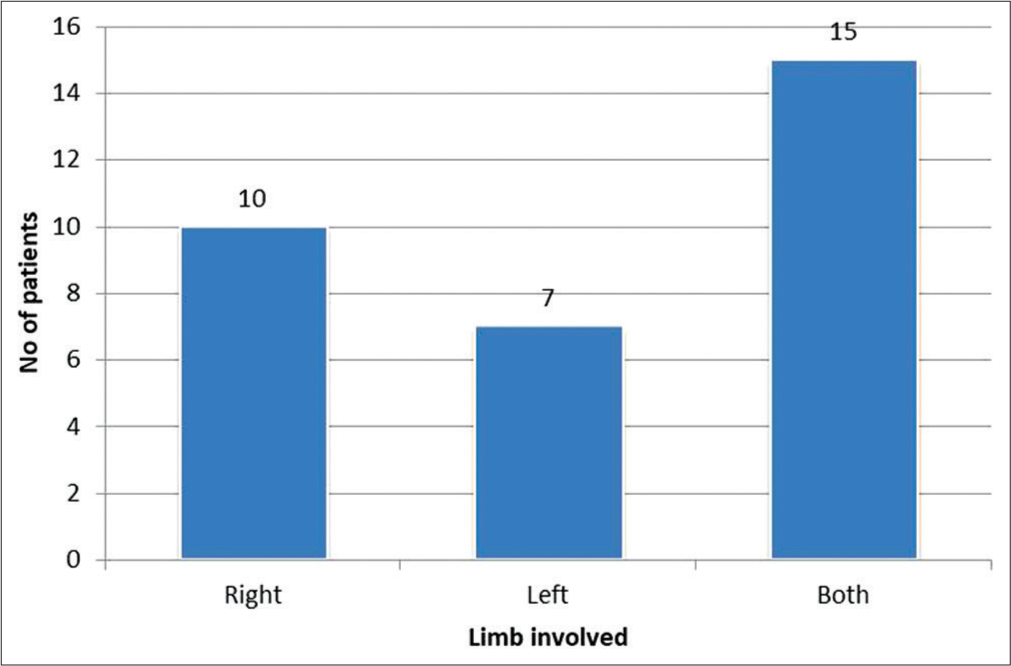
In our study, the VCSS tool was useful to study the changes in the clinical scores; we could efficiently validate the changes in the clinical presentation and the evolving remedy responses. Koyano and Sakaguchi studied the VCSS and found good correlation among all severity scores, especially among CEAP scores and VCSS.[10] In our study of patients with varicose veins the number percentage of male patients were 44% and the number percentage of females were 56% [Figure 1] the number of patients with right leg involvement was 10 and number of patients with left leg was 7 and the number of patients with bilateral involvement was 15 [Figure 2]. We assessed the score severity distribution before and after treatment; most cases improved [Figure 3]. The VCSS showed marked improvement; the left leg improved in 20 patients and remained the same in 5 [Figure 4], while the right leg improved in 16 patients and remained the same in 6. In the left leg, the pre-and post-treatment mean score was 6.32 ± 5.32 and post score was 3.91 ± 2.47, respectively [Table 1]. From the doppler study out of the 22 patients with right leg involvement, only 5 improved and the remainig 17 remained same and in the left leg out of 25 patients with left leg involvement, 7 improved and 18 remained same [Figure 5]. The mean change in the score was 2.41 ± 3.83, indicating 38.13% improvement, which is statistically highly significant (P = 0.008). In the right leg, the pre- and post-treatment mean score was 4.84 ± 2.59 and 3.04 ± 2.23, respectively [Table 2]. The mean change was 1.80 ± 1.66 indicating a 37.19% improvement, which is statistically highly significant (P = 0.000) 5.53 ± 4.1 and 3.45 ± 2.36, respectively. The cumulative pre- and post-treatment score was 5.53 ± 4.15 and 3.45 ± 2.36, respectively [Table 3]. The mean change was 2.09 ± 2.87, indicating a 37.69% improvement (P = 0.000) [Table 4].
- Distribution of cases according to sex.
- Distribution of cases according to the limb involvement.

- Severity distribution–venous clinical severity score (before and after).

- Venous clinical severity score outcome.

- Doppler outcome.
| n | Mean | Std. Deviation | Median | Mean change | SD of change | Change (%) | t-value | P-value | |
|---|---|---|---|---|---|---|---|---|---|
| L | |||||||||
| Pre-score | 22 | 6.32 | 5.37 | 5.00 | 2.41 | 3.83 | 38.13 | 2.95 | 0.008 HS |
| Post-score | 22 | 3.91 | 2.47 | 3.00 |
VCSS: Venous clinical severity score
| n | Mean | Std. Deviation | Median | Mean change | SD of change | Change (%) | t-value | P-value | |
|---|---|---|---|---|---|---|---|---|---|
| R | |||||||||
| Pre-score | 25 | 4.84 | 2.59 | 4.00 | 1.80 | 1.66 | 37.19 | 5.43 | 0.000 HS |
| Post-score | 25 | 3.04 | 2.23 | 3.00 |
VCSS: Venous clinical severity score
| n | Mean | Std. Deviation | Median | Mean change | SD of change | Change (%) | t-value | P-value | |
|---|---|---|---|---|---|---|---|---|---|
| Total | |||||||||
| Pre-score | 47 | 5.53 | 4.15 | 5.00 | 2.08 | 2.87 | 37.69 | 4.99 | 0.000 HS |
| Post-score | 47 | 3.45 | 2.36 | 3.00 |
VCSS: Venous clinical severity score
| Association between VCSS and Doppler | Side | Chi-square value | ||||
|---|---|---|---|---|---|---|
| L | R | Total | ||||
| Count | Count | Count | ||||
| VCCS Score | Result scale | Improved | 16 | 20 | 36 | P=0.000, HS (improved) |
| Not improved | 6 | 5 | 11 | |||
| Total | 22 | 25 | 47 | |||
| Doppler | Result scan | Improved | 5 | 7 | 12 | P=0.001, HS (not improved) |
| Not improved | 17 | 18 | 35 | |||
| Total | 22 | 25 | 47 | |||
VCSS: Venous clinical severity score
DISCUSSION
Out of 60 patients enlisted and selected for the study, 32 completed the study [Table 5]. Among these 32, 18 (56%) were men and 14 (44%) were women [Figure 1]. This is in accordance with a study from the UK wherein 60% or patients with varicose veins were men, although women more often present themselves for treatment.[11]
| Reg no | VCSS | |||||
|---|---|---|---|---|---|---|
| Right | Left | |||||
| Pre-score | Post-score | Result | Pre-score | Post-score | Result | |
| DVV1 | – | – | 7 | 6 | Improved | |
| DVV2 | – | – | 11 | 6 | Improved | |
| DVV4 | 2 | 3 | Not Improved | – | – | |
| DVV6 | 10 | 10 | Status quo | 9 | 9 | Status quo |
| DVV7 | – | – | 24 | 9 | Improved | |
| DVV8 | 9 | 4 | Improved | – | – | |
| DVV10 | – | – | 5 | 3 | Improved | |
| DVV14 | 5 | 3 | Improved | 5 | 3 | Improved |
| DVV17 | 5 | 1 | Improved | – | – | |
| DVV18 | 3 | 3 | Status quo | 2 | 2 | Status quo |
| DVV19 | 5 | 2 | Improved | – | – | |
| DVV21 | 4 | 4 | Status quo | – | – | |
| DVV23 | 3 | 5 | Not–Improved | 2 | 5 | Not Improved |
| DVV25 | 2 | 0 | Improved | 2 | 1 | Improved |
| DVV27 | 7 | 4 | Improved | 7 | 3 | Improved |
| DVV28 | 4 | 3 | Improved | 3 | 2 | Improved |
| DVV30 | 1 | 0 | Improved | 2 | 5 | Not Improved |
| DVV32 | – | – | 15 | 6 | Improved | |
| DVV33 | 6 | 4 | Improved | – | – | |
| DVV35 | 4 | 2 | Improved | – | – | |
| DVV36 | 7 | 4 | Improved | – | – | |
| DVV38 | – | – | 8 | 4 | Improved | |
| DVV40 | 3 | 2 | Improved | 3 | 2 | Improved |
| DVV43 | 3 | 1 | Improved | – | – | |
| DVV45 | – | – | 5 | 2 | Improved | |
| DVV47 | 3 | 1 | Improved | – | – | |
| DVV48 | 3 | 1 | Improved | 1 | 1 | Status quo |
| DVV49 | 8 | 6 | Improved | 7 | 5 | Improved |
| DVV51 | 6 | 4 | Improved | 3 | 1 | Improved |
| DVV54 | 3 | 2 | Improved | 5 | 2 | Improved |
| DVV56 | 11 | 6 | Improved | 11 | 7 | Improved |
| DVV59 | 4 | 1 | Improved | 2 | 2 | Status quo |
VCSS: Venous clinical severity score
Most patients had lesions in both legs. In our study, the right leg was affected in ten patients, the left in seven, and both legs were affected in 15 patients [Figure 2]. However, Shenoy reported a higher occurrence of left leg involvement.[12] A research study by Joseph et al. states that veins on the left side were more involved than on the right.[13]
The selection of Hamamelis as the choice of remedy is supported by mentions in homoeopathic literature. A recent study by Hooda and Tripathi on the role of homoeopathic remedies in varicose veins states that Hamamelis is an essential remedy for varicose veins and venous ulcers.[14] Devi and Aathi also reported the use of Hamamelis ×3 every 3 hours when the veins are affected.[15]
While surgery minimizes varicose veins, it is not a fool proof answer. Michaels et al. state that varicose veins may reoccur due to neovascularization, even after thorough surgery, or they may develop elsewhere in the leg.[16]
The most likely reason for no improvements seen on the Doppler study was the short duration of treatment and short interval between successive scans.
CONCLUSION
From the present study, we can conclude that Hamamelis is an effective remedy for the treatment of varicose veins and its complications, based on the significant improvement in the VCSS after treatment. However, there was no change or improvement in the Doppler study reports, most likely due to the short duration of the study. In future, studies with larger patient groups and longer follow-up duration are required to produce more in-depth and useful data.
Acknowledgments
Special thanks to Professor Sucharitha Suresh MSc (statistics), Department of Community Medicine, Father Muller Medical College, Mangalore.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
The authors thank and acknowledge the financial support provided by the Rajiv Gandhi University of Health Sciences, Bengaluru, and Karnataka.
Conflicts of interest
There are no conflicts of interest.
References
- Compression treatment of chronic venous insufficiency In: Handbook of Venous Disease. New York: Arnold; 2001. p. :303-8.
- [Google Scholar]
- Study of clinical features and management of varicose veins of lower limb. J Clinic Diagn Res. 2011;5:1416-20.
- [Google Scholar]
- Available from: https://www.en.wikipedia.org/wiki/Witch-hazel [Last accessed on 2021 May 03]
- Hemorrhoids and varicose veins: A review of treatment options. Alternat Med Rev. 2001;6:126.
- [Google Scholar]
- Lectures on Homoeopathic Materia Medica New Delhi: B Jain Pub Pvt Ltd.; 1984. p. :564.
- [Google Scholar]
- Revision of the venous clinical severity score: Venous outcomes consensus statement: Special communication of the American venous forum ad hoc outcomes working group. J Vascular Surg. 2010;52:1387-96.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized clinical trial of endovenous laser ablation versus conventional surgery for small saphenous varicose veins. J Vascular Surg. 2015;61:834.
- [CrossRef] [PubMed] [Google Scholar]
- Selective stripping operation based on Doppler ultrasonic findings for primary varicose veins of the lower extremities. Surgery. 1988;103:615-9.
- [Google Scholar]
- Lifestyle factors and the risk of varicose veins: Edinburgh vein study. J Clin Epidemiol. 2003;56:171-9.
- [CrossRef] [Google Scholar]
- Shenoy A, ed. Manipal Manual of Surgery. Tamil Nadu: CBS Publishers and Distributors; 2014.
- A multicenter review of epidemiology and management of varicose veins for national guidance. Ann Med Surg. 2016;8:21-7.
- [CrossRef] [PubMed] [Google Scholar]
- Role of homeopathy medical system in remedy of varicose vein ulcer. Int J Homoeop Sci. 2018;2:29-31.
- [Google Scholar]
- Randomised clinical Trial, Observational Study and Assessment of Cost-effectiveness of the Treatment of Varicose Veins (REACTIV trial), Southampton. UK: NIHR Health Technology Assessment Programme: Executive Summaries 2006
- [CrossRef] [PubMed] [Google Scholar]