Translate this page into:
A case report on the impact of homoeopathic intervention in psychosis
*Corresponding author: S. Karunakara Moorthi, Department of Psychiatry, National Homoeopathy Research Institute in Mental Health, Kottayam, Kerala, India. dr.karunakaramoorthi@gmail.Com
-
Received: ,
Accepted: ,
How to cite this article: Karunakara Moorthi S, Pertin S, Nithin R. A case report on impact of homoeopathic intervention in psychosis. J Intgr Stand Homoeopathy. 2024;7:70-7. doi: 10.25259/JISH_44_2023
Abstract
Psychosis refers to losing contact with reality, during which hallucinations or delusions may occur. A 62-year-old woman reported in the Outpatient Department with symptoms of psychosis for one month. The consultant psychiatrist diagnosed it as a case of Unspecified Nonorganic Psychosis (F29). The Brief Psychiatric Rating Scale (BPRS) score was 55 at the time of the initial consultation. Lachesis Muta 30 was selected as the Individualised Homoeopathic Medicine. It helped to taper the conventional medicines, as well as it was possible to withdraw the medication gradually. BPRS score was reduced to 18 within four months. Modified Naranjo criteria were used to assess whether the changes were likely associated with the homoeopathic intervention. Overall, improvement was noticed clinically and in BPRS. In this case, individualised homoeopathic treatment has shown a positive role in the management and treatment of psychosis as an add-on therapy.
Keywords
Psychosis
Delusions
Homoeopathy
Lachesis
Brief Psychiatric Rating Scale
INTRODUCTION
Psychosis is defined as a mental disorder in which the thoughts, affective response, ability to recognise reality, and ability to communicate and relate to others are sufficiently impaired to interfere grossly with the capacity to deal with reality; the classical characteristics of psychosis are impaired reality testing, hallucinations, delusions, and illusions.[1]
Moreno-Küstner et al. suggests that the descriptive results of the pooled median global prevalence of psychotic disorders were 4.6/1000 persons, while the median point and 12-month prevalence was 3.89 and 4.03/1000 persons, respectively, and the median lifetime prevalence was 7.49/1000 persons.[2]
A study conducted in Kerala suggests that the prevalence of psychosis was 0.7%.[3] As per National Mental Health Survey (NMHS) 2015–2016, the age group between 40 and 49 years was predominantly affected. The gender prevalence of psychotic disorders was nearly similar (lifetime: male: 1.5%; female: 1.3%; current: male: 0.5% and female: 0.4%). Residents from urban metros had a greater prevalence across the different disorders. Data from the NMHS reveal that mental disorders were significantly higher in households with lesser income, poor education and limited employment.[4]
Psychotic disorders are associated with substantial premature mortality,[5,6] morbidity[7], and a large social and financial burden.[8] The economic cost of care for a person with a mental disorder, mainly as out-of-pocket expenditure, reveals a huge burden, while the hidden and intangible costs are difficult to monetise.[4] Socioeconomic deprivation, inequality, and instability are also associated with increased incidence.[9,10]
Antipsychotics are considered the first-line agents for acute and maintenance therapy of psychotic disorders. It can be of great benefit in a range of psychiatric disorders, including schizophrenia and bipolar disorder, but all are associated with a wide range of potential adverse effects. These can impair quality of life, cause stigma, lead to poor adherence to medication, cause physical morbidity, and, in extreme cases, be fatal.[11] Second-generation antipsychotics (SGAs) or atypical antipsychotics were considered to be more effective and safer than typical or first-generation antipsychotics (FGAs).[12-15] Many studies have concluded that olanzapine, risperidone, clozapine, and pooled SGAs caused significantly less extrapyramidal side effects akathisia than FGAs but showed larger weight gain and caused metabolic syndromes than FGA comparators.[16-18]
Thus, the limitations of existing antipsychotic drugs to alleviate all of the pathologic dimensions of the illness (i.e., negative symptoms, cognitive deficits, and social disabilities) have produced awareness that no single treatment may be sufficient. There is a need for an alternative treatment that will do more good than harm or one that can be used adjunctively with antipsychotic drugs.
The Brief Psychiatric Rating Scale (BPRS) is one of the most frequently used instruments for evaluating psychopathology in patients with psychotic disorders. It was developed in the early 1960s by John E.Overall and Donald R Gorham, using factor analysis. It is designed to assess the severity of psychotic states, with the aim of providing clinicians a way to quickly assess changes in the patient’s mental status. Each of the 18 items is designed to represent a discrete symptom area. Items are rated on a 7-point Likert scale, from 1 = ‘not present’ to 7 = ‘extremely severe,’ with scores ranging from 18 to 126 (achieved through summing the item scores).[19]
Homoeopathy is a therapeutic method that has proved useful in many psychiatric conditions involving psychosis. There are published papers that show the usefulness of homoeopathy as a stand-alone treatment as well as an add-on treatment, which shows marked improvement.[20-22]
We report a case involving a woman of age 62 years who was diagnosed with psychosis not otherwise specified (NOS). The outcome was assessed with the help of BPRS scale in every follow-up visit.
The patient visited the psychiatry outpatient department (OPD) of a tertiary care hospital in Kerala with complaints that met the criteria of psychosis on the basis of the International Classification of Diseases, Tenth Revision (ICD-10) Diagnostic Criteria for Research.
Consent was obtained from the caregiver. Case taking was done followed by analysis and evaluation of the symptoms with framing of the totality of the symptoms. Synthesis repertory was preferred, and using Radar Opus software, repertorisation was done. Medicine was selected after referring to Materia Medica, based on the very prominent presenting complaints and generals of the patient. A single medicine was prescribed, as and when required with a minimum dose. Assessment of the symptom severity was done by BPRS with the help of the Consultant Psychiatrist of the Institution. The BPRS was assessed every month. The assessment of BPRS is shown in Table 1. The Modified Naranjo Criteria for Homoeopathy– Causal Attribution Inventory was used for assessing the likelihood of a causal relationship between a homoeopathic intervention and clinical outcome. It is shown in Table 2. The strength of association between the medicine and outcome was assessed by the following criteria: definite: ≥9; probable 5–8; possible 1–4 and doubtful ≤ 0.[23]
| Domains | 1st follow-up | 2nd follow-up | 3rd follow-up | 4th follow-up | 5th follow-up | 6th follow-up | 7th follow-up | 8th follow-up | 9th follow-up | 10th follow-up | 11th follow-up | 12th follow-up | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Somatic concern | 6 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| 2. Anxiety | 6 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | ||
| 3. Emotional withdrawal | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| 4. Conceptual organisation | 5 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| 5. Guilt feelings | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| 6. Tension | 6 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | ||
| 7. Mannerisms and posturing | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| 8. Grandiosity | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| 9. Depressive mood | 4 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | ||
| 10. Hostility | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| 11. Suspiciousness | 6 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 4 | 1 | 1 | 1 | ||
| 12. Hallucinatory behaviour | 6 | 4 | 3 | 2 | 1 | 1 | 1 | 1 | 4 | 1 | 1 | 1 | ||
| 13. Motor retardation | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| 14. Uncooperativeness | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| 15 Unusual thought content | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| 16. Blunted affect | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| 17. Excitement | 4 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | ||
| 18. Disorientation | 3 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| Total Score | 55 | 26 | 20 | 19 | 18 | 18 | 18 | 18 | 28 | 18 | 18 | 18 | ||
BPRS: Brief psychiatric rating scale
| S. No. | Criteria | Yes | No | Not sure | Case |
|---|---|---|---|---|---|
| 1. | Was there an improvement in the main symptom or condition for which the homoeopathic medicine was prescribed? | +2 | -1 | 0 | +2 |
| 2. | Did the clinical improvement occur within a plausible time frame relative to the drug intake? | +1 | -2 | 0 | +1 |
| 3. | Was there an aggravation of symptoms? | +1 | 0 | 0 | 0 |
| 4. | Did the effect encompass more than the main symptom or condition, i.e., were other symptoms ultimately improved or changed? | +1 | 0 | 0 | +1 |
| 5. | Did overall well-being improve? | +1 | 0 | 0 | +1 |
| 6. | (A) Direction of cure: Did some symptoms improve in the opposite order of the development of symptoms of the disease? |
+1 | 0 | 0 | 0 |
| (B) Direction of cure: Did at least two of the following aspects apply to the order of improvement of symptoms: - from organs of more importance to those of less importance - from deeper to more superficial aspects of the individual - from the top downward |
+1 | 0 | 0 | 0 | |
| 7. | Did ‘old symptoms’ (defined as non-seasonal and non cyclical symptoms that were previously thought to have resolved) reappear temporarily during the course of improvement? | +1 | 0 | 0 | +1 |
| 8. | Are there alternate causes (other than the medicine) that – with a high probability – could have caused the improvement? (Consider known course of disease, other forms of treatment, and other clinically relevant interventions) |
-3 | +1 | 0 | 0 |
| 9. | Was the health improvement confirmed by any objective data? (BPRS). | +2 | 0 | 0 | +2 |
| 10. | Did repeat dosing, if conducted, create similar clinical improvement? | +1 | 0 | 0 | 0 |
BPRS: Brief psychiatric rating scale
After improvement started, the patient was put on a placebo. Repetition of medicine was done according to the principles of homoeopathy.
CASE REPORT
A woman of age 62 years came with complaints of sleeplessness, self-talking, fearfulness, hearing voices of neighbors and undue suspicions that people were talking about her, weeping spells, and frequent hurling of abuses at neighbors. She was showing increased religiosity and also had a poor appetite for a month.
History of presenting complaints
The patient did not have any psychiatric illness till 47 years of age. Her complaints had started suddenly on a fateful night when she went to the barn to render assistance to a cow, in giving birth. While she was waiting there for the cow to go into labour, she saw a flurry of grotesque images flashing before her eyes and became petrified. The next day, she left her house to a neighbour’s house with a knife in her hand. She was immediately brought to a nearby hospital and was given depot preparations. She was admitted to the hospital for a month and discharged with marked improvement. She had been on regular medications for five years, and thereafter, she was under irregular medication for seven years. Her complaints gradually reappeared when she was without medications. Her family started noticing behavioral changes in her, such as self-talking, sleeplessness, hurling abuses at neighbours, and restlessly walking to and fro in the house with the belief that people were talking bad about her. Once again, she was taken to a hospital and was admitted there for a week. She continued medication for three years and was apparently doing well, but there has been a significant increase in her symptoms since a month, she was hospitalised, and her dose of regular medication was increased to no alleviation of her complaints.
She used to lie on the bed without sleeping. Sometimes, she would walk here and there and chant prayers. She has a fearful expression on her face. She frequently complained that people are talking about her and were doing things against her. Hence, she was brought to our hospital and was under the following medications Tab. Sizodon plus (1/2-0-1), Tab Quetiapine 100 mg (0-0-1) and Tab Ativan (0-0-1).
History of past illness
Chicken pox – Childhood, took folk medicine.
Chikungunya – 13 years ago, took allopathic treatment.
Family history
Father deceased at 75 years from bronchial asthma. Mother has hypertension and type II diabetes mellitus. Husband died at 59 years of age from myocardial infarction. The younger brother died from accidental drowning. There is no family history of psychiatric illness.
Life space investigation
The patient hails from a middle-class family in Kerala. She was the eldest in the family among six siblings. Father worked as daily wage labour in a merchant shop, and mother was a homemaker. She had quite a normal upbringing. Her parents lived peacefully without any discord. She shared a good bond with her parents and all her siblings. She was more of an extrovert. She studied up to 10th standard but failed in her exams and did not pursue further studies. She got married at the age of 28 years. Her husband worked as a labourer in a Rubber estate while she looked after their two children. Her husband was an alcoholic, but they lived together without any issues. He died nine years ago from a heart attack.
Physical generals
Her appetite was poor, and her thirst was increased. Her perspiration was scanty. She has sleeplessness. She attained menopause at the age of 49 years. She has a desire for fish and vegetables. Thermally, she is a hot patient.
Clinical findings (Mental status examination baseline)
General appearance and behaviour: Conscious, aware of her surroundings, help-seeking, moderately kempt, hair not properly combed, nail short trimmed, lean built, and rapport: established easily.
Eye to eye contact: Maintained
Interpersonal relationship: Poor
Psychomotor activity: No Abnormality Detected (NAD)
Speech: Rate of speech: Increased
Affect: Appropriate
-
Mood: Subjective: fearful
Objective: fearful
-
Thoughts:
Flow: Increased
Form: NAD
Content: Delusion of reference, delusion of persecution
-
Perceptual disorder:
Hallucinations: Auditory – second person hallucination Illusions: NAD
-
Orientation to: Time – Poor
Place – Poor
Person – Good
Memory: Good
General Information and Intelligence: Average
Attention and concentration: Poor
Abstract thinking: Poor
Judgement:
Social judgement: Average
Test judgement: Average
Insight: Complete denial of illness.
Timeline
The mental status examination of the case for the 3rd, 6th, 9th, and 12th months is depicted in Table 3. The follow-up of the case is depicted in Table 4.
| S. No. | Domains | 3rd months | 6th months | 9th months | 12th months |
|---|---|---|---|---|---|
| 1. | General appearance and behaviour | Well-dressed, rapport established | Well-dressed, rapport established | Well-dressed, rapport established | Well-dressed, rapport established |
| 2. | Psychomotor activity | NAD | NAD | NAD | NAD |
| 3. | Speech | ||||
| Rate | Normal | Normal | Normal | Normal | |
| Volume | Normal | Normal | Normal | Normal | |
| Reaction time | Normal | Normal | Normal | Normal | |
| Tone | Normal | Normal | Normal | Normal | |
| 4. | Affect | Appropriate | Appropriate | Appropriate | Appropriate |
| 5. | Mood | Fearfulness: Markedly reduced | Fearfulness: Markedly reduced | Fearful as earlier | Fearfulness: Markedly reduced |
| 6. | Thoughts | ||||
| Flow | NAD | NAD | NAD | NAD | |
| Form | NAD | NAD | NAD | NAD | |
| Content | Delusion of reference and persecution: Reduced | Delusion of reference and persecution: Moderately reduced | Delusion of reference and persecution: Reappeared as earlier | Delusion of reference : Markedly reduced Delusion of persecution : Nil | |
| 7. | Perceptual disorder | ||||
| Hallucinations | Nil | Nil | Occasional auditory hallucinations | Nil | |
| Illusions | Nil | Nil | Nil | Nil | |
| 8. | Orientation | Well-oriented | Well-oriented | Well-oriented | Well-oriented |
| 9. | Memory | Intact | Intact | Intact | Intact |
| 10. | Attention and concentration | Improved | Improved | Improved well | Improved well |
| 11. | Abstract thinking | Poor | Poor | Poor | Good |
| 12. | Judgement | Average | Average | Average | Average |
| 13. | Insight | Grade 1 | Grade 1 | Grade 3 | Grade 3 |
NAD: No abnormality detected.
| S. No. | Date | Symptoms | Allopathic prescription | Homoeopathic prescription |
|---|---|---|---|---|
| 1. | 04/07/2020 | Sleeplessness, hearing voices of neighbour, fear, self-talking, weeping spells, verbal abusiveness, reduced appetite. | T. Sizodonplus (1/2-0-1/2) T. Quitipin 100mg (0-0-1) T. Ativan (0-0-1) |
Lachesis 30/4 Doses, weekly once |
| 2. | 18/07/2020 | Sleep-adequate, Auditory hallucination-reduced, self-talking-reduced, No weeping, No hurling of abuses. | T. Sizodon plus (0-0-1/2) T. Quitipin 50mg (0-0-1) T. Ativan (0-0-1) |
Sac Lac/10 Doses, 3 days once. |
| 3. | 18/08/2020 | Sound sleep, auditory hallucination: markedly reduced, no self-talking, no weeping, no abusiveness. | T. Sizodon plus (0-0-1/2) T. Quitipin 50mg (0-0-1/2) T. Ativan (0-0-1) |
Lachesis 30/4 Dose (S.O.S). Advised to take weekly once, if needed. |
| 4. | 13/10/2020 | Patient feels much better, sleeping well, auditory hallucination: Markedly reduced, no self-talking, no weeping tendency, fear: Reduced. Two doses of SOS were needed to be taken. | T. Sizodon plus (0-0-1/2) T. Quitipin 50mg (0-0-1/2) |
Sac Lac/10 Doses, 3 days once |
| 5. | 24/11/2020 | General improvement of all complaints. Sound sleep, good appetite, SOS not taken. | T. Sizodon plus (0-0-1/2) | Sac Lac/10 Doses, 3 days once |
| 6. | 26/12/2020 | Patient feels much better | T. Sizodon plus (0-0-1/2) | Sac Lac/10 Doses, 3 days once |
| 7. | 28/01/2021 | No other new or old complaints, doing household work, sound sleep, no fear. | No allopathic medication. | Sac Lac/10 Doses, 3 days once |
| 8. | 23/03/2021 | Patient feels much better | No allopathic medication | Sac Lac/10 Doses, 3 days once |
| 9. | 20/04/2021 | Talk to self, hearing voice (2PAH), fear and suspiciousness toward neighbours, anxious about her son, doing household work. Sleep-disturbed occasionally. | No allopathic medication | Lachesis 30/4 Doses, weekly once. |
| 10. | 21/05/2021 | Self-talk-reduced, 2PAH-reduced, No fear, anxiety and suspiciousness. Sleep improved. | No allopathic medication | Lachesis 30/4 Doses (S.O.S). Advised to take weekly once, if needed. |
| 11. | 23/06/2021 | General relief of all complaints. 4 doses of SOS were taken. |
No allopathic medications | Lachesis 30/4 Doses (S.O.S). Advised to take weekly once, if needed. |
| 12. | 04/07/2021 | No self-talking, Hearing voice-nil, Tension-nil, no fear, anxiety or undue suspicions. Adequate sleeping hours. SOS not taken. | No allopathic medication | Lachesis 30/4 Doses (S.O.S). Advised to take weekly once, if needed. |
The patient is still continuing regular OPD follow-ups. No psychotic symptoms were reported. She has been fully functional in family. Occasionally, we prescribe Lachesis to prevent any deterioration to the previous state, SOS: Si opus sit.
As per the complaints, findings of mental status examination, and the consultant psychiatrist of the institution, the patient was diagnosed as suffering from Unspecified Non-organic Psychosis (F 29) as per the ICD-10 Diagnostic Criteria of Research.[24] It needs to be differentiated from schizophrenia, psychotic type of mood disorders, and persistent delusional disorder. Since the symptoms of the patient do not meet the ICD-10 criteria for diagnosis of schizophrenia, the diagnosis of schizophrenia is ruled out.
In the psychotic type of mood disorder, the course of the disease will be episodic, and there will be a prominent disturbance of mood along with the psychotic symptoms of schizophrenia.
In delusional disorder, the behaviour of the patient will be normal, apart from having psychotic symptoms. Clear and persistent auditory hallucination rules out the diagnosis of delusional disorder in this case.
Therapeutic intervention
Individualised homoeopathy medicine was administered to the patient. Lachesis 30CH was prescribed to the patient.
DISCUSSION
Through years of hard work and experience, Hahnemann in Organon of Medicine has laid down the pivotal guidelines for the treatment and management of mental diseases in aphorisms 210–230.[25] The causative factor for this case is explained under the aphorism 221. To get complete recovery, the patient must be treated with homoeopathic anti-psoric drugs for long periods. However, since the patient was treated with conventional medicines for a long period, we could not get the exact picture. Hence, with the available presenting symptoms, repertorial totality was erected. A few disease symptoms were also added for repertorisation. This was done to confirm that individualistic medicine is similar to the disease as well. The remedy was selected after consultation with Homoeopathic Materia Medica. Repertorisation chart is shown in Figure 1. Lachesis came up first in the repertory chart, followed by Hyoscyamus niger and Veratrum album.
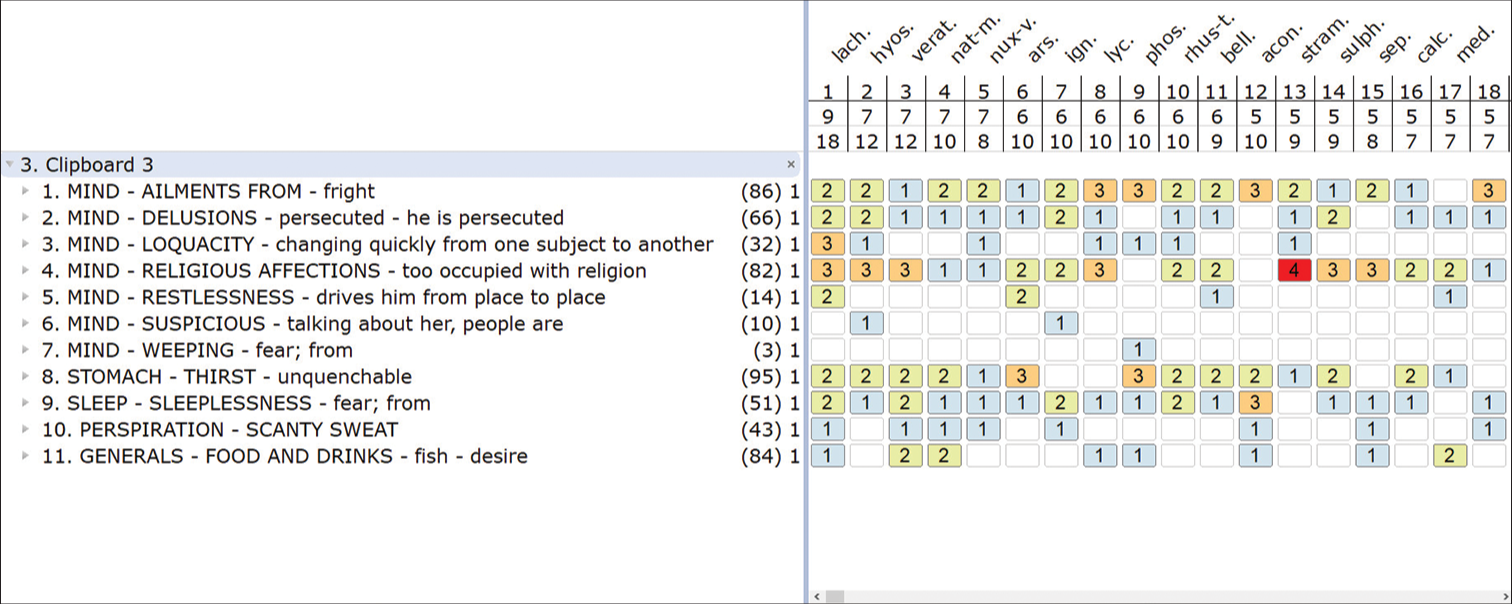
- Repertorial chart.
The prominent features such as paranoia, restlessness, fear, sleeplessness, increased religiosity, loquacity, and hot thermal state were sustained for prescribing Lachesis. Even though H. niger is also suspicious and talkative. The important characteristics and symptoms such as obscenity, foolish talk as well as behaviour and great hilarity were not present in the patient. More boost up for prescription of V. album symptoms such as obsession in religiosity and punctuality, quarrelsome rigid and haughty expression, cutting and tearing mania, howling, screaming, preaching, and uncertain fear of death were not present.[26,27]
The case is of long-standing duration with marked psychotic symptoms and abnormal behaviour. The disease had affected her familial and social interpersonal relationships and functioning. After the homoeopathic intervention, she feels symptomatic relief as well as there is improvement in the social and familial relationships also.
During the course of treatment, the anti-psychotic medication which the patient had been taking for years was tapered. Complete withdrawal from conventional medicine was possible within six months of add-on homoeopathic intervention. BPRS was used to assess the outcome of the homoeopathic intervention by comparing the reading before and after the intervention. A BPRS score of 55 at baseline was reduced to a score of 18 with homoeopathic intervention. The patient reported slight exacerbation of the symptoms at the 9th month of follow-up, which was managed with homoeopathic intervention alone. The patient is religiously coming to the OPD for monthly follow-ups.
CONCLUSION
The case report is aimed to show that homoeopathy can enhance the quality of life, and reduce the financial burden as well as mental discomfort of patients suffering from psychotic disorders, without the aid of conventional medication.
The present case report evidently suggests the successful treatment of psychosis and improving quality of life, and restoration of the well-being of the patient with the help of individualised homoeopathic medicine. This case has highlighted the importance of a holistic approach in the treatment considering the individuality of a patient and the use of repertorisation for the remedy selection, and not just disease symptoms. However, it would not be appropriate to generalise the usefulness of homoeopathy in cases of psychosis on the basis of a single case report. Therefore, rigorous observational and high-quality randomised control studies with larger sample sizes are suggested to ascertain the result obtained in the present case report.
Acknowledgments
The authors are thankful to Dr. K.C. Muraleedharan, Officer In-charge, and Dr. N. D. Mohan, H.O.D Department of Psychiatry. They are also obliged to the participant and the caregivers for their valuable input, which made the study possible.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Synopsis of psychiatry: Behavioral sciences clinical psychiatry United States: Williams and Wilkins Co; 1988.
- [CrossRef] [Google Scholar]
- Prevalence of psychotic disorders and its association with methodological issues. A systematic review and meta-analyses. PLoS One. 2018;13:e0195687.
- [CrossRef] [PubMed] [Google Scholar]
- Psychiatric morbidity in the community: A population based study from Kerala. Indian J Psychiatry. 2017;59:149-56.
- [CrossRef] [PubMed] [Google Scholar]
- National Mental Health Survey of India, 2015-16: Prevalence, patterns and outcomes Bengaluru: National Institute of Mental Health and Neuro Sciences Publication; 2016. p. :129.
- [Google Scholar]
- Mortality gap for people with bipolar disorder and schizophrenia: UK-based cohort study 2000-2014. Br J Psychiatry. 2017;211:175-81.
- [CrossRef] [PubMed] [Google Scholar]
- Years of potential life lost and life expectancy in schizophrenia: A systematic review and meta-analysis. Lancet Psychiatry. 2017;4:295-301.
- [CrossRef] [PubMed] [Google Scholar]
- Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789-858.
- [CrossRef] [PubMed] [Google Scholar]
- The global costs of schizophrenia. Schizophr Bull. 2004;30:279-93.
- [CrossRef] [PubMed] [Google Scholar]
- Poverty, inequality and the treated incidence of first-episode Psychosis: An ecological study from South Africa. Soc Psychiatry Psychiatr Epidemiol. 2008;43:331-5.
- [CrossRef] [PubMed] [Google Scholar]
- Mental disorders in urban areas: An ecological study of schizophrenia and other psychoses Chicago: University of Chicago Press; 1939.
- [Google Scholar]
- Treatment of psychosis: 30 years of progress. J Clin Pharm Ther. 2006;31:523-34.
- [CrossRef] [PubMed] [Google Scholar]
- A meta-analysis of the efficacy of second-generation antipsychotics. Arch Gen Psychiatry. 2003;60:553-64.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of second generation antipsychotics: A systematic review of randomized trials. BMC Psychiatry. 2008;8:31.
- [CrossRef] [PubMed] [Google Scholar]
- A meta-analysis of head-to-head comparisons of second-generation antipsychotics in the treatment of schizophrenia. Am J Psychiatry. 2009;166:152-63.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of individual second-generation vs. first-generation antipsychotics in first-episode Psychosis: A systematic review and meta-analysis. Int J Neuropsychopharmacol. 2013;16:1205-18.
- [CrossRef] [PubMed] [Google Scholar]
- Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: A systematic review and meta-analysis. Schizophr Res. 2010;123:225-33.
- [CrossRef] [PubMed] [Google Scholar]
- Second-generation antipsychotics and metabolic side effects: A systematic review of population-based studies. Drug Saf. 2017;40:771-81.
- [CrossRef] [PubMed] [Google Scholar]
- Metabolic and hormonal side effects in children and adolescents treated with second-generation antipsychotics. J Clin Psychiatry. 2008;69:1165-75.
- [CrossRef] [PubMed] [Google Scholar]
- Available from: https://www.smchealth.org/sites/main/files/file-attachments/bprsform.pdf [Last accessed on 2023 May 29]
- Homoeopathic treatment for severe depression with psychotic features: A case report. Int J Homoeopath Sci. 2020;4:82-6.
- [CrossRef] [Google Scholar]
- Usefulness of individualised homoeopathic medicine in Manic episode-A case report. Indian J Res Homoeopathy. 2021;15:41.
- [CrossRef] [Google Scholar]
- Homoeopathic management of Schizophrenia: A prospective, non-comparative, open-label observational study. Indian J Res Homoeopathy. 2016;10:108-18.
- [CrossRef] [Google Scholar]
- Homeopathic clinical case reports: Development of a supplement (HOM-CASE) to the CARE clinical case reporting guideline. Complement Ther Med. 2016;25:78-85.
- [CrossRef] [PubMed] [Google Scholar]
- The ICD-10, classification of mental and behavioural disorders New Delhi: AITBS Publishers and Distributors; 2007.
- [Google Scholar]
- New manual of homoeopathic materia medica and repertory with repertory (3rd ed). New Delhi: B. Jain Publishers Ltd.; 2007. p. :297-585.
- [Google Scholar]