Translate this page into:
Individualised homoeopathy in the treatment of hyperuricaemia: A single-arm clinical trial
*Corresponding author: Dr. Abhijit Dutta, Department of Organon of Medicine, National Institute of Homoeopathy, Kolkata, West Bengal, India. drabhijitdutta1@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Debnath P, Ali SA, Dutta A. Individualised homoeopathy in the treatment of hyperuricaemia: A single-arm clinical trial. J Intgr Stand Homoeopathy. 2024;7:97-101. doi: 10.25259/JISH_13_2024
Abstract
Objectives:
Hyperuricaemia is a metabolic disorder characterised by abnormally high levels of uric acid in the blood, which can lead to gout, kidney stones, and cardiovascular disease. While some studies have suggested that homoeopathic remedies may be effective in reducing uric acid levels and improving symptoms in patients with hyperuricaemia, there is limited scientific evidence to support their use as a primary treatment.
Material and Methods:
An open-label, prospective, non-controlled, and pre-post comparison clinical trial was conducted on 30 patients diagnosed with hyperuricaemia to assess the effect of individualised homoeopathic medicines after 3 months of treatment. Eligible patients were aged between 20 and 65 years, of both sexes and had a serum uric acid level >6 mg/dL in women and >7 mg/dL in men. Patients taking urate-lowering agents were excluded from the study. Serum uric acid level was used as the primary outcome measure.
Results:
The study found that homoeopathic treatment was associated with a significant reduction in serum uric acid levels (mean difference ± standard error: −2.04 ± 0.16, P < 0.001) after 3 months of treatment. There were no reported adverse effects associated with the treatment.
Conclusion:
This clinical trial provides preliminary evidence to support the potential effect of homoeopathic treatment for hyperuricaemia. However, further research with larger sample sizes and more rigorous study designs is needed to confirm these findings and determine the optimal use of homoeopathy in the management of hyperuricaemia.
Keywords
Hyperuricaemia
Homoeopathy
Serum uric acid
INTRODUCTION
Hyperuricaemia is a medical condition characterised by abnormally high uric acid levels in the blood. Uric acid is a waste product formed during the breakdown of purines, which are found in many foods and produced by the body.[1] Normally, uric acid dissolves in the blood and is eliminated from the body through urine. However, when the body produces too much uric acid, or if the kidneys are unable to eliminate it efficiently, the excess uric acid can form crystals in the joints, causing painful inflammation and leading to a condition termed gout.[2] Hyperuricaemia has also been linked to other health problems, such as kidney stones and cardiovascular disease.[3]
Hyperuricaemia is a common metabolic disorder affecting millions of people worldwide. The prevalence of hyperuricaemia varies across populations and is influenced by genetic, lifestyle, and dietary factors. Men are more likely to develop hyperuricaemia than women, and the incidence increases with age.[4]
According to the National Health and Nutrition Examination Survey, approximately 21% of US adults had hyperuricaemia in 2007–2008, and the prevalence increased with age, affecting over 40% of adults aged 75 years and older.[5] Hyperuricaemia is also more common in certain ethnic groups, with higher rates reported in African Americans and Pacific Islanders compared to other populations.[6] The condition is strongly associated with other comorbidities such as metabolic syndrome, obesity, hypertension, and chronic kidney disease. Moreover, lifestyle factors such as alcohol consumption, a high purine diet, and low physical activity levels are known to increase the risk of hyperuricaemia.[1]
The prevalence of hyperuricaemia has increased in recent years, possibly due to diet and lifestyle changes. This rise in incidence has raised concerns about the potential health consequences of hyperuricaemia, including gout, kidney stones, and cardiovascular disease. These factors have led to increased interest in developing effective interventions for managing hyperuricaemia, to reduce its associated health risks.[7]
Homoeopathy is an alternative medicine based on the principle of “like cures like.” It involves using highly diluted substances that would produce symptoms similar to the patient’s condition in a healthy person to stimulate the body’s natural healing processes. While there is some anecdotal evidence that homoeopathy may be effective for certain conditions, the scientific evidence for its use in hyperuricaemia is limited.[8]
Some studies have investigated the use of homoeopathy for hyperuricaemia, but the results have been mixed. One study published in 2012 found that the homoeopathic remedy Benzoicum acidum was effective in reducing uric acid levels in patients with hyperuricaemia. However, this study was small and had several limitations, including a lack of a control group and a short follow-up period.
Another study by Nayak et al.[9] evaluated the efficacy of individualised homoeopathy (IH), Urtica urens mother tincture, and both, along with lifestyle modifications, in a sample of 90 patients with hyperuricaemia. Although all three therapies showed similar improvements, the group receiving both IH and U. urens mother tincture had more positive outcomes than either of the individual interventions. However, this study was also small and had some methodological limitations. Overall, there is currently not enough scientific evidence to support the use of homoeopathy as a primary treatment for hyperuricaemia. Therefore, this study was conducted as a pilot trial to understand the effect of homoeopathic medicines when administered as individualised therapy.
MATERIAL AND METHODS
Trial design
An open-label, prospective, non-controlled, and pre-post-comparison clinical trial was conducted on 30 patients diagnosed with hyperuricaemia to assess the effect of homoeopathic treatment. The participants were recruited at the Outpatient Department of the National Institute of Homoeopathy, Kolkata, India. The study protocol was approved by the Institutional Ethics Committee (Ref. F. No. 5-23/NIH/PG/Ethical Comm.2009/Vol 5/2603[A/S], dt. 6 March 2018). The trial protocol and full dissertation were submitted as a post-graduate thesis by the primary author to the West Bengal University of Health Sciences, Kolkata, India.
Eligibility criteria
The inclusion criteria for this study were patients with hyperuricaemia with its consequences, aged 20–65 years, of both sexes, of all religions, and of different socioeconomic statuses. The serum uric acid level should be >6 mg/dL in women and >7 mg/dL in men. Patients must agree to give consent for participating in the study and to comply with the protocol.
The exclusion criteria for the study were patients taking urate-lowering agents, those unwilling to participate, those who do not undergo regular follow-up and discontinue treatment for personal reasons, severe or advanced cases requiring surgical procedures or orthopaedic correction, patients unwilling to undergo any investigation if so advised, those reluctant to undergo physical activity, exercise, and low purine food habit, patients who are mentally retarded and taking psychotropic drugs, chronic alcoholism, and pregnant or lactating women.
Intervention
The planned intervention involved the administration of homoeopathic remedies on centesimal and 50 millesimal scales. For the centesimal scale, each dose consisted of 4–6 cane sugar globules (no. 10) that were moistened with the indicated medicine (preserved in 90% v/v ethanol) and taken orally on a clean tongue and empty stomach. The dosage and repetition were tailored to the individual requirements of the case. However, for the 50 millesimal scale, one no. 10 globule was dissolved in 120 mL distilled water, with 5–10 drops of rectified spirit added and mixed well to make 16 doses, which were to be taken orally on an empty stomach, every alternate day for 1 month (with successive increase of potency in the next months). Duration of therapy: 3 months.
Lifestyle modification (LSM) was recommended for all the patients. LSM was advised in terms of encouraging a lacto-vegetarian diet; restriction or moderation of high purine content food, for example, meat, fish, poultry, organ meat, oyster, seafood, yeast and yeast extracts, cauliflower, mushroom, lentils, spinach, beans and peas; moderation of alcohol consumption; adequate fluids (2 L/day); hot or cold compress over the affected joint; rest in bed and immobilisation of the affected joint in acute gout; moderate exercise in chronic gout; physiotherapy and counselling and patient education.
Outcome measures
Primary: Serum uric acid level measured at the baseline and after 3 months
Secondary: Any adverse event during the study.
Sample size
Due to the preliminary nature of the study, a conventional sample size of 30 was decided.
Statistical technique and data analysis
Baseline descriptive data (categorical and continuous) were depicted using absolute values, percentages, means, standard deviations, medians, and interquartile ranges. An intention-to-treat approach was followed, meaning that every included patient was entered into the final analysis, and missing values were replaced by the last observation carried forward method. Data distribution was examined using the Kolmogorov– Smirnov test and Shapiro–Wilk test. The changes in serum uric acid levels before and after treatment were evaluated at baseline and after 3 months using a parametric t-test (due to the normally distributed data). Statistical significance was set at 0.05. Data analysis was conducted using IBM® Statistical Package for the Social Sciences Statistics for Windows, version 26 (IBM Corp., Armonk, NY, USA).
RESULTS
Participant flow
Based on the inclusion and exclusion criteria mentioned earlier, a total of 41 patients with hyperuricaemia were screened. Out of these, 11 patients were excluded for different reasons, while the remaining 30 fulfilled the eligibility criteria and were included in the study [Figure 1]. Sociodemographic and outcome data were collected from the patients before the intervention, and after 3 months, the outcome data were recorded once again.
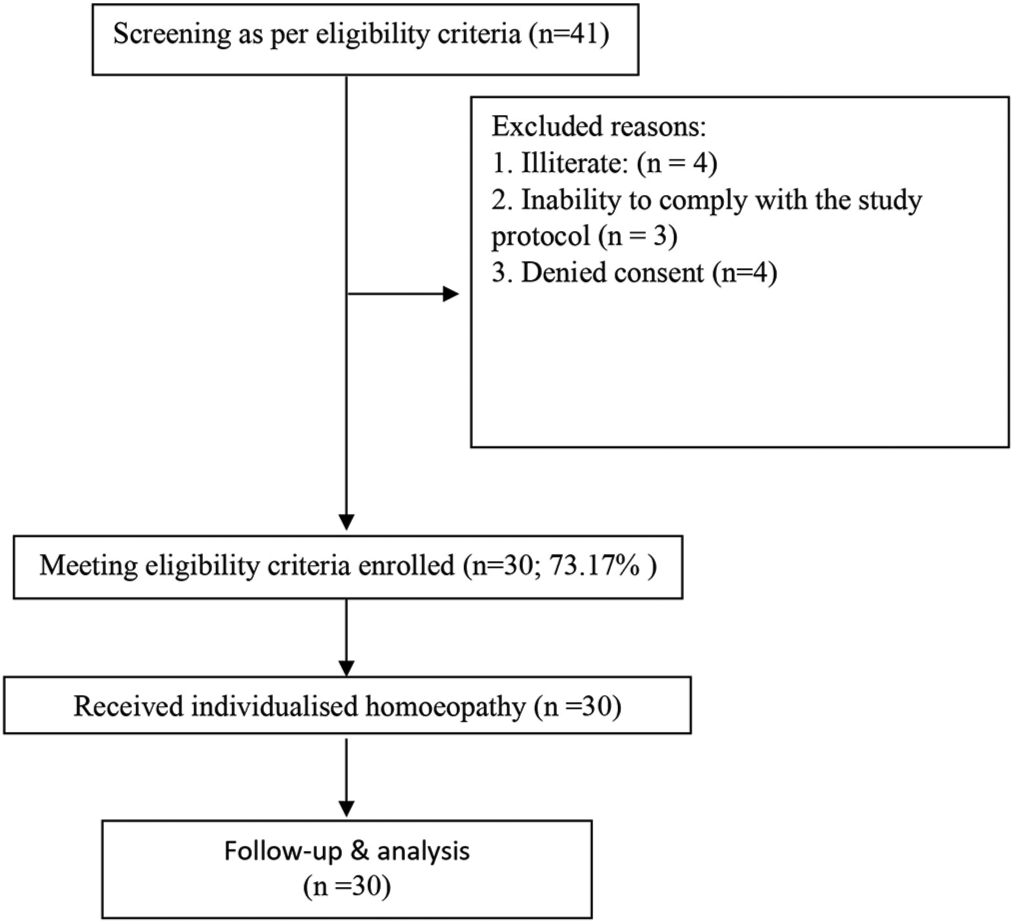
- Selection of participants.
Recruitment
The study was started in March 2018, and the follow-up of the last enrolled patient was completed by the end of January 2019.
Baseline data
During the 18-month study period, a total of 30 patients (18 males and 12 females) were enrolled as per the inclusion and exclusion criteria and were followed up and studied. Fourteen variables were considered: Age, sex, religion, marital status, residence, socioeconomic status, education, employment, food habits, treatment taken, co-morbidities, body mass index, systolic blood pressure, and diastolic blood pressure [Table 1].
| Variable | Value |
|---|---|
| Age, µ±SD | 49.5±9.7 |
| Sex , n(%) | |
| Male | 18 (60.0) |
| Female | 12 (40.0) |
| Religion , n(%) | |
| Hindu | 23 (76.7) |
| Islam | 7 (23.3) |
| Residence , n(%) | |
| Rural | 13 (43.3) |
| Urban | 17 (56.7) |
| Education , n(%) | |
| Up to Class X | 18 (60.0) |
| Up to Class XII | 8 (26.7) |
| Graduate or above | 4 (13.3) |
| Employment , n(%) | |
| Service | 7 (23.3) |
| Business | 10 (33.3) |
| Unemployed | 13 (43.3) |
| Income status , n (%) | |
| <10,000/Month | 21 (70.0) |
| 10,000–20,000/Month | 5 (16.7) |
| >20,000/Month | 4 (13.3) |
| Food habit , n(%) | |
| Veg | 0 (0.0) |
| Non-veg | 30 (100.0) |
| Marital status , n (%) | |
| Unmarried | 2 (6.7) |
| Married | 28 (93.3) |
| Treatment taken , n (%) | |
| Allopathy | 20 (66.7) |
| Homoeopathy | 5 (16.7) |
| No such | 2 (6.7) |
| Comorbidities , n (%) | |
| Arthritis | 5 (16.7) |
| Chronic gastritis | 4 (13.3) |
| Diabetes | 4 (13.3) |
| Hypertension | 3 (10) |
| Others | 12 (40) |
| None | 2 (6.7) |
| BMI, µ±SD | 25.2±3.6 |
| SBP (in mm of Hg), µ±SD | 127.36±11.78 |
| DBP (in mm of Hg), µ±SD | 81.33±8.63 |
N.B.- µ: Mean, SD: Standard deviation, n: Number, %: Percentage, BMI: Body mass index, SBP: Systolic blood pressure, DBP: Diastolic blood pressure
Numbers analysed
Outcomes from 30 subjects were complete; therefore, all the enrolled subjects (n = 30) entered the final analyses.
Data distribution
The data were found to be a normal distribution which was found using the Kolmogorov – Smirnov test and the Shapiro–Wilk test, which both produced P-values more than 0.05. Thus, it was intended to conduct a parametric two-tailed, paired sample t-test.
Outcomes and estimation
A statistically significant reduction was achieved in the serum uric acid level before and after intervention (two-tailed paired sample t-test, P < 0.001) [Table 2].
| Outcome measure | Baseline µ±SD | After 3 months µ±SD | Difference MD±SE | t-value | P-Value |
|---|---|---|---|---|---|
| Serum uric acid,mg/dL | 7.4±0.75 | 5.35±0.89 | −2.04±0.16 | −12.48 | <0.001* |
µ: Mean, SD: Standard deviation, MD: Mean difference, SE: Standard error, The P<0.05* was considered as significant
Medicines used
Thirteen different medicines were used in the study at different time points. The two most frequently prescribed medicines were Lycopodium clavatum (23.3%), Medorrhinum (16.7%), and Thuja occidentalis (13.3%). In 70% of cases, the Centesimal potency was used; the 50 millesimal in 30% [Table 3].
| Prescribed medicine | n(%) |
| Lycopodium clavatum | 7 (23.3) |
| Medorrhinum | 5 (16.7) |
| Thuja occidentalis | 4 (13.3) |
| Bryonia alba | 2 (6.7) |
| Calcarea carbonicum | 2 (6.7) |
| Natrum sulphuricum | 2 (6.7) |
| Rhus toxicodendron | 2 (6.7) |
| Arnica Montana | 1 (3.3) |
| Carcinosinum | 1 (3.3) |
| Causticum | 1 (3.3) |
| Lachesis mutus | 1 (3.3) |
| Pulsatilla nigricans | 1 (3.3) |
| Sulphur | 1 (3.3) |
| Prescribed potency | n(%) |
| Centesimal | 9 (30) |
| 50 millesimal | 21 (70) |
Adverse events
There were no reported serious adverse effects associated with the treatment.
DISCUSSION
The paper discusses a clinical trial evaluating the effectiveness of a novel treatment approach for hyperuricaemia, which is a medical condition characterised by abnormally high levels of uric acid in the blood.[3] The prevalence of hyperuricaemia has been increasing worldwide, and there is a need for effective interventions to manage this condition.[7] Homoeopathy is an alternative medicine based on the principle of “like cures like” and involves using highly diluted substances that would produce symptoms similar to the patient’s condition in a healthy person to stimulate the body’s natural healing processes. The study aimed to assess the effect of homoeopathic treatment on patients diagnosed with hyperuricaemia. The study was an open-label, prospective, non-controlled, and pre-post-comparison clinical trial conducted on 30 patients diagnosed with hyperuricaemia to assess the effect of homoeopathic treatment. The principal finding of the study was that IH resulted in a statistically significant reduction in uric acid levels in patients with hyperuricaemia.
In this study, the sample size was relatively small (30 patients), and the trial was open-label and non-controlled, which could introduce bias and limit the ability to draw causal inferences. The lack of a control group and blinding means that the observed changes in uric acid levels could be due to other factors, such as a placebo effect, natural fluctuations in uric acid levels, or changes in diet or lifestyle. In addition, the duration of the study was relatively short (12 weeks), which may not be long enough to fully evaluate the efficacy and safety of the intervention. Therefore, while the study provides some preliminary data on the use of IH for hyperuricaemia, the limitations of the study design and small sample size suggest that further research is needed to fully evaluate the efficacy and safety of this intervention.
A previous study by Nayak et al.[9] investigated the use of homoeopathy for hyperuricaemia, but the results were mixed. The study evaluated the comparative effect of IH, U. urens mother tincture and both in reducing serum uric acid levels. However, this study has several methodological issues, including the open-label design, small sample size, and inconclusive results.
Further, research with larger sample sizes and controlled designs is needed to fully evaluate the efficacy and safety of homoeopathy for hyperuricaemia.
CONCLUSION
The results of this pilot study suggest that IH may be a promising approach for managing hyperuricaemia. However, given the limitations of the study, further research is needed to confirm these findings and determine the long-term effects of homoeopathic treatment on hyperuricaemia and its associated health risks. Future studies could use a larger sample size, randomised controlled design, and longer follow-up periods to provide more robust evidence of the effectiveness of homoeopathy for hyperuricaemia. In addition, future research could investigate the mechanisms by which homoeopathic remedies may exert their effects on uric acid levels, as well as explore the potential use of homoeopathy as an adjunctive therapy to standard pharmacological treatments for hyperuricaemia. Overall, this study provides a foundation for further research into the use of homoeopathy for managing hyperuricaemia and highlights the need for more rigorous clinical trials in this area.
Ethical approval
The research/study approved by the Institutional Ethics Committee (IEC) Board at National Institute of Homoeopathy, Kolkata, India, number F. No. 5-23/NIH/PG/Ethical Comm.2009/Vol 5/2603(A/S), dated 06 March 2018.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Hyperuricemia. 2022. Available from: http://www.ncbi.nlm.nih.gov/books/NBK459218 [Last accessed on 2024 Feb 19]
- [Google Scholar]
- Uric acid, hyperuricemia and vascular diseases. Front Biosci. 2012;17:656-69.
- [CrossRef] [PubMed] [Google Scholar]
- The epidemiology and genetics of hyperuricemia and gout across major racial groups: A literature review and population genetics secondary database analysis. J Pers Med. 2021;11:231.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of gout and hyperuricemia in the US general population: The National Health and Nutrition Examination Survey 2007-2008. Arthritis Rheum. 2011;63:3136-41.
- [CrossRef] [PubMed] [Google Scholar]
- Racial and gender disparities among patients with gout. Curr Rheumatol Rep. 2013;15:307.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of hyperuricemia and its related risk factors in healthy adults from Northern and Northeastern Chinese provinces. BMC Public Health. 2013;13:664.
- [CrossRef] [PubMed] [Google Scholar]
- Controlled clinical studies of homeopathy. Homeopathy. 2015;104:328-32.
- [CrossRef] [PubMed] [Google Scholar]
- Individualized homeopathic medicines and Urtica urens mother tincture in treatment of hyperuricemia: An open, randomized, pragmatic, pilot trial. J Complement Integr Med. 2021;18:599-608.
- [CrossRef] [PubMed] [Google Scholar]