Translate this page into:
Executing and assessing programme for mental well-being in an old age home during the COVID-19 pandemic by a homoeopathic institution: Challenges and outcomes
*Corresponding author: Dr. Mansi Surati, Department of Psychiatry, Dr. M. L. Dhawale Memorial Homoeopathic Institute, Palghar, Maharashtra, India. mansi.surati@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Surati M, Patel MK, Nikumbh SB, Yadav RR, Kukde AD, Nigwekar AM, et al. Executing and assessing programme for mental well-being in an old age home during the COVID-19 pandemic by a homoeopathic institution: Challenges and outcomes. J Intgr Stand Homoeopathy 2022;5:86-92.
Abstract
Objective:
COVID-19 pandemic has affected the provision of psychiatric care across the world and the elderly have been the most disadvantaged. Psychological stress in them is not only due to excess mortality risk but also due to restrictions instituted to mitigate the chances of contracting COVID. The current pandemic is likely to lead to substantial changes in the health-care services as it has shown the need for improved multidisciplinary and community- centered care. The purpose of this paper is to address the challenges faced while implementing a multidisciplinary structured programme for the mental well-being in residents of old age home and assess the role played by the sustainable multidisciplinary structured interventions to alleviate the psychological suffering. The old age home in the study is situated in a remote area of Palghar district. Availing of required medical health-care facility during a pandemic was a challenge in itself, where delivering the multidisciplinary intervention for mental well-being was a much needed and never tested in such a setup.
Material and Methods:
Primary screening and knowledge of acute and chronic stressors revealed the current status of emotional wounds and hence the emotional sensitivity of the group. Scales (generalised anxiety disorder [GAD-7], patient health questionnaires [PHQ-2] and dementia assessment by rapid test [DART]) were employed to evaluate intensity of anxiety, depressive symptoms and dementia. Techniques to deal with distress demonstrated in each session were based on action learning principles. Structured group interventions were done through relevant videos, group discussions, relaxation techniques, meditation and physical exercise by the team of homoeopathic physicians, psychologist and physiotherapist. Results were subjected to statistical analysis.
Results:
There was a statistically significant reduction in anxiety following intervention, z = −3.886, P < 0.001, with a large effect size (r =.57). The median score on the anxiety decreased from 10 to 4 in a span of 10 months. No significant improvement was found in physical health and cognitive impairment.
Keywords
Cognitive impairment
Relaxation techniques
Mindfulness
Multidisciplinary approach
Holistic homoeopathic care
INTRODUCTION
Problem description
The old age home (OAH) mentioned in this study is situated in a remote area of Palghar district. Availing of required medical health-care facilities during the COVID-19 pandemic was a challenge in itself. In such a setup, delivering the multidisciplinary approach model of mental well-being was a much needed and never tested intervention.
In a paper published in 2021, the process of structuring the mental well-being programme through a team-led multidisciplinary approach based on action learning principles is spelt out in detail.[1] The present article outlines the challenges encountered in the execution of these interventions and evidence-based assessment of the outcome.
Irrespective of living arrangements and place of stay, psychiatric morbidity among elderly people is common, severe and multifaceted. Community-based studies reported the prevalence of depression and cognitive impairment among the elderly to be 47.0% and 43.25%, respectively. Low socioeconomic status, loss of spouse, living alone, chronic comorbidities, cognitive impairment, bereavement and restricted activities of daily living were significant risk factors for depression.[2] To address these, multiple clusters of mental health professionals have collaborated with non-government organisations to set up helplines and provide free mental health counselling.[3]
A study of psychiatric and physical morbidity in OAHs in Southern India found the prevalence of psychiatric disorders to be 44.14%; the prevalence in women (44.4%) being slightly higher than that in men (43.6%). Depression was the most common psychiatric disorder (26.2%), followed by anxiety (10.34%) and dementia (7.6%).[4] A secondary record analysis was conducted on 2308 geriatric patients seen from 2000 to 2010 at Dr. M. L. Dhawale Memorial Trust’s Rural Homoeopathic Hospital, Palghar. A majority were between 60 and 65 years of age; 9.35% sought homoeopathic treatment for general medical complaints, 4.41% for psychiatric complaints, 39.8% for skeletal affections, 9.96 for respiratory complaints and 9.74% for gastrointestinal tract disorders.[5] Clinical profiling of 1015 patients admitted for psychiatry in-patient care at the Dr. M. L. Dhawale Rural homoeopathic Hospital in Palghar (2014–2018) showed that 35% had alcohol withdrawal, 12.7% had conversion reaction, 9.8% had attempted and 9.7% had anxiety.[6]
A study conducted in OAHs from four districts of Northern India on 306 inmates selected through purposive sampling indicated that the average prevalence of mental health problems among the elderly was 41.3% in the community and 64.4% in old age homes. The study showed greater prevalence in women (51%) than in men (28%). Depression (37.7%) was found to be the most common mental health problem, followed by anxiety (13.3%) and dementia (11.1%).[7]
During the first wave of COVID-19, a study had been conducted to assess the psychological burden among the elderly residing at OAHs. It was found that 23.9% of residents had become anxious and nervous, 19% felt more depressed and 9% had unspecified insomnia. The study indicated that the more severe the degree of infection in the area, the more likely was the increase in the residents’ adverse psychological state.[8]
Several studies show that homoeopathy can be effective in all age groups with anxiety or depression. A study of patients 20–60 years of age revealed that individualised homoeopathy showed significant results in reducing anxiety symptoms.[9] A prospective and unicentric study showed that individualised homoeopathic treatment resulted in significant improvement in depressive symptoms in the 20–60 years age group. Natrum muriaticum, Arsenic album, Pulsatilla nigricans, Lycopodium clavatum and Phosphorus were the remedies chiefly used; the depressive symptoms were assessed using the Hamilton depression rating scale, Beck depression inventory and the clinical global impressions scale.[10]
There are few scientific studies on the impact of homoeopathy on dementia.[11] However, a pilot feasibility study on an adapted mindfulness intervention for people with dementia in care homes revealed significant improvement in quality of life in the intervention group. Their methodology included ten sessions focused on intervention plus modern pharmacological medication in mild-to-moderate dementia.[12] A quasi-experimental study on the effectiveness of the structured group reminiscence therapy in decreasing loneliness, depressive symptoms and anxiety in an OAH in the Chittor district also found a reduction of depressive rating; however, the difference was not statistically significant.[13]
PHQs are common screening tools for mental health disorders. The PHQ–2, introduced in 2003, specifically targets depressive symptoms.[14] The seven-item GAD-7 screening was developed to screen GAD-7 in the primary setting. Psychometric evaluation with the GAD-7 suggests that it is a reliable and valid measure of GAD symptoms in the psychiatric and general population.[15] The DART has been developed based on clinical observations in the outpatient Clinical Neuropsychology department of the All India Institute of Medical Sciences, New Delhi. It consists of four items selected as per domains affected in dementia and mild cognitive impairment following the DSM-5. It is widely used in clinical and epidemiological research internationally and in India.[16]
Aim and objectives
Aim
Assessing existing mental health morbidity and implementing and assessing planned interventions in residents of an OAH during the COVID-19 pandemic.
Objectives
The objectives were as follows:
Identifying the prevalence of mental health morbidity among residents of an OAH during the COVID-19 pandemic to plan/modify planned interventions
Addressing operational issues in the effective implementation of a structured and holistic mental well-being programme
Assessing the role of such an intervention with a view to replicate such programs for the elderly in other OAHs.
MATERIAL AND METHODS
Context
The study was carried out on the same population described in the study conducted by Surati, et al. in 2021.[1] However, language barrier, awareness about self and vocalising one’s own experiences were some of the challenges to implementing these themes. This required modification in planning the interventions. [Tables 1-5] describe the study population, its characteristics and the operational issues identified and modifications done when implementing structured group therapy.
| Age | Percentage | Prevalence of physical comorbidity |
|---|---|---|
| 60–70 years | 17 | 19 |
| 70–80 years | 42 | 50 |
| 80–90 years | 33 | 31 |
| 90–100 years | 4 | 0 |
| Parameters | Present (n=16) | Absent (n=7) | P-value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Age | 76.69 | 6.77 | 74.00 | 17.67 | 0.922 |
| PHQ-2 | 2.63 | 2.44 | 2.71 | 2.28 | 0.671 |
| GAD-7 | 10.69 | 6.17 | 10.86 | 4.88 | 0.922 |
| DART | 1.69 | 0.71 | 1.86 | 1.06 | 0.671 |
DART: Dementia assessment by rapid test, GAD-7: Generalised anxiety disorder, PHQ-2: Patient health questionnaires
* Mann–Whitney U-Test applied at 95% confidence interval, significant if P ≤ 0.05.
| Before Intervention | After Intervention | P value | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Median | Mean | SD | Median | |
| PHQ-2 | ||||||
| 2.65 | 2.347 | 2.00 | 2.22 | 1.808 | 2.00 | 0.496 |
| GAD-7 | ||||||
| 10.74 | 5.699 | 10.00 | 5.22 | 5.648 | 4.00 | 0.000 |
| DART | ||||||
| 1.74 | 0.810 | 2.00 | 1.91 | 0.996 | 2.00 | 0.570 |
DART: Dementia assessment by rapid test, GAD-7: Generalised anxiety disorder, PHQ-2: Patient health questionnaires
Wilcoxon signed-rank test applied at 95% CI, significant if P value ≤ 0.05, **P=0.00024
| Sr. no | Themes of modules | Qualitative responses post intervention |
|---|---|---|
| 1 | Understanding mood | - One of the most introverted residents became emotional and spoke about the inspiration he got from the character in the movie and a fresh perspective to deal with his internal struggle - An elderly lady who had similarly lost her son, as in the movie clip, became emotional but found strength to fight her grief - Group discussion helped residents to vent out which enabled the group to be more concerned and caring for each other and more respectful toward individual struggles |
| 2 | Handling anger and frustration | One of the residents could grasp her frustration resulting from her unpleasant past and its impact on present relationships. She expressed a desire to be more forgiving and valuing of the relations developed in the OAH. Insight regarding her own behaviour helped to understand the distress she went through. |
| 3 | Emotional well-being | One of the residents who had never held a pen in his hand, sketched for the first time and felt it engaging and expressed desire to repeat it whenever he felt lonely. |
| 4 | Handling fear and anxiety | Role play could bridge the gap and brought acceptance of their anxious thoughts and resultant behaviour. Engagement was observed followed by acceptance and the solutions were discussed. |
| 5 | Identifying depression | Sharing and communication as an effective measure to deal with sadness. Residents who hardly spoke with each other in the past 4–5 years realised the effectiveness of communication in releasing tension |
| 6 | Forgetfulness and dementia | One of the residents was a known case of Dementia. Insight that his behaviour of blaming people for his stolen items was not intentional but stemming from disease was understood. Group discussed dealing with his forgetfulness, blames and his anger |
| 7 | Being physically active | Active session on group exercise made them feel energetic and fresh. This provided the motivation to engage in exercise sessions conducted weekly |
| 8 | Art of graceful ageing | Entire group became active and engaged very well and promised to maintain the resolution that gave them joy. A resident who was a ‘visharad’ in music (a formal qualification in study of Indian music) promised to sing and another resident promised to engage everyone in yoga, thereby facilitating small group activities |
| 9 | Power of meditation | Most of them felt empowered since it was performed in the group. They showed willingness to perform group meditation once in a week |
| 10 | Group dynamics | Most of them consciously realised that they had formed their new family in the OAH and felt gratitude toward each other for being there through thick and thin |
OAH: Old age home
| Sr. No | Themes of modules | Operational issues | Techniques used to overcome |
|---|---|---|---|
| 1 | Understanding Mood | - Language Barrier - Initiating group discussion |
- The video was selected without audio. It was a short movie named ‘Blue Helmet’ depicting a story of a mother living independently after her son’s death in a road traffic accident. Wearing a helmet, she protects herself from every subtle injury – even at home. A helmet is symbolic of how one protects brooding. Self-care and independent living in old age was depicted - Using regional language and avoiding scientific terms helped. |
| 2 | Handling anger and frustration | - Bringing acceptance of having anger and its roots lying in past | -Self-disclosure of the subject expert on his anger pattern helped the group to look within |
| 3 | Emotional well-being | Convincingly demonstrate to them the effectiveness of techniques for bringing in well-being, for example, Grounding technique, painting/sketching | Pre-and post-intervention emotional states were tapped in presence of the entire group |
| 4 | Handling fear and anxiety | Difficulty in identifying what they experienced as anxiety and accepting pre-occupation with anxious thoughts | Indirect demonstration through role plays depicting everyday scenarios of anxious behaviours of residents. The help of care givers was taken to acquire information about their daily behaviour |
| 5 | Identifying depression | Demonstrate the relevance of the activity to identify the emoticons based on the partners’ moods and to explain them the reason behind the colours the choose. | - Scale was used, which reflected their overall experience of staying in an OAH - Findings of the scales were corelated with their mood and resultant selection of colours |
| 6 | Forgetfulness and dementia | - Destroying the myth that forgetfulness and dementia are same - Blaming others for lost time in dementia patients is intentional |
- Subject expert shared multiple examples of her forgetfulness - Corelated same with group member’s forgetfulness - Finally, shared a case of dementia in detail and corelated with behaviour of the dementia patient from the group itself |
| 7 | Being physically active | A subject expert was diagnosed with COVID and required the immediate arrangement of a competent specialist | A physiotherapist was called for the topic. |
| 8 | Art of graceful aging | The selected video was in English. | The issue was solved using regional language and replicating the conversation with a group as in the video. It turned out to be an engaging conversation |
| 9 | Power of meditation | - No issues were faced | |
| 10 | Group dynamics | - No issues were faced |
OAH: Old age home
Sample size: The sample size was 11 men and 13 women.
Interventions
Objectives for each module were set out with the techniques based on action learning principles. Relaxation technique, grounding technique, mindfulness exercise and evolving group discussions were used.
Measures
Instruments Utilised:
The residents were screened; physical and mental complaints were recorded by the team, taking note of acute and chronic stressors to aid holistic understanding
Assessment of psychiatric illness was done by applying the PHQ-2, GAD-7 and DART. These were administered by PG residents, the study co-ordinator and the psychologists to assess the prevalence of mental morbidity and to test the effectiveness of interventions at 6-month intervals.
Statistical analysis was done using SPSS 24.0 version.[17] The Wilcoxon signed-rank test was applied to understand the impact of the interventions as the data were qualitative and measured in ordinal form. The post-study assessment was delayed by 3–4 months, since 17 of the OAH residents in the study were diagnosed with COVID.
Ethical considerations
All relevant consents were taken.
RESULTS
A total of 23 patients were considered for analysis. One of the resident was taken back home by the relatives; hence, the number reduced from 24 sample population to 23.
The medical comorbidities included diabetes mellitus, hypertension, bronchial asthma and arthritis. The highest number of comorbidities was in the 70–80 years age group (50%) followed by the 80–90 years age group (31%).
Grief was the predominant stressor, caused by death of close ones (44%), anxious disposition (13%), betrayal (4%) and abandonment by family (22%) [Figure 1].
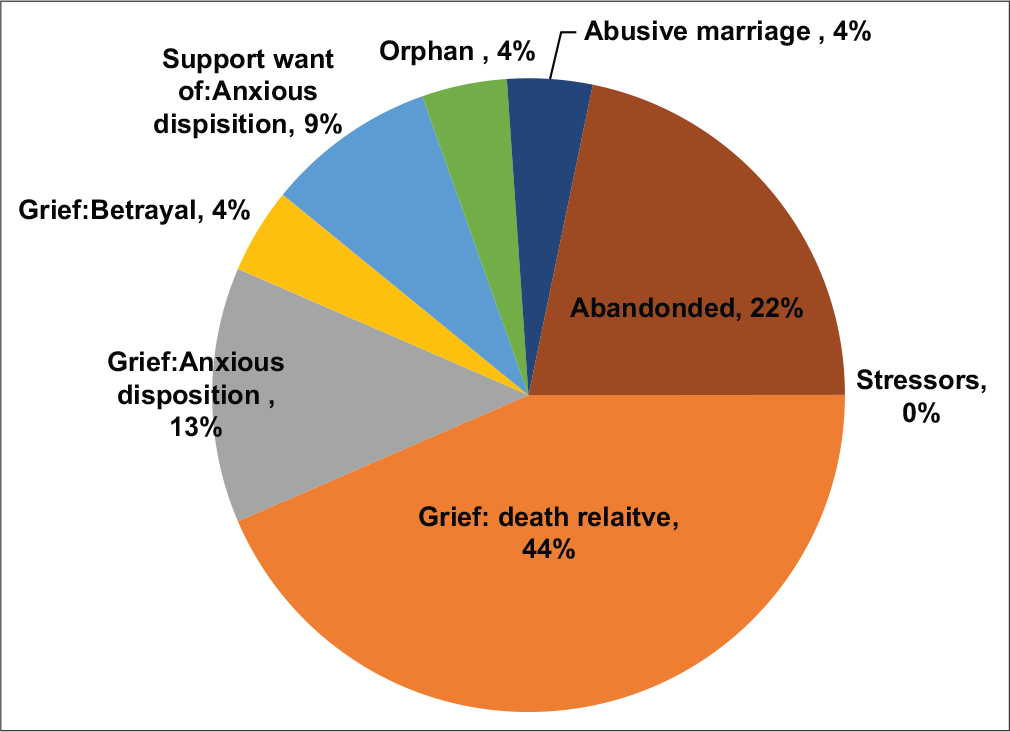
- Prevalence of stressors.
Since the residents were already under homoeopathic treatment, some had been prescribed homoeopathic medicines for anxiety, including arsenic album, gelsemium and pulsatilla nigricans. In case of grief due to loss of loved ones, remedies such as ignatia amara, natrum mur and phosphorus were prescribed.
An attempt was made to study if the state of physical comorbidities had any influence on the outcome of the interventions. Since P values are >0.05, the presence of comorbidities did not influence study outcomes.
The Wilcoxon signed-rank test revealed a statistically significant reduction in anxiety following intervention, z = −3.886, P < 0.001, with a large effect size (r = 0.57). The median score on anxiety decreased from 10 to 4 in a span of 10 months
The Wilcoxon signed-rank test did not reveal any statistically significant improvement in physical health quality and cognition following the intervention, z = −.681, P = 0.496 and z = −.568, P = 0.570, respectively. Indeed, median score before and after intervention in a span of 359 ± 11.12 days shows no deterioration as well.
Qualitative assessment of the intervention
The table below highlights the operational issues and ways, in which they were overcome yielding a qualitative response in the session.
DISCUSSION
Significant reduction in anxiety was found in our study population. Anxiety about the future and about health was the most common expression. Since most of the residents did contract COVID-19, it triggered anxiety. However, medical assistance provided by the OAH authorities and care received from fellow residents and caretakers did give them a feeling of security and gratitude. Regular practice of Yoga, relaxation, breathing exercises and becoming aware of various shades of anxiety helped in the alleviation of complaints. Residents those were on homoeopathic medicines before COVID was prescribed remedies such as arsenic album, gelsemium and pulsatilla nigricans for anxiety episodes. Residents with significant grief were administered remedies such as ignatia, natrum mur and phosphorus. While depressive symptoms showed improvement (2.65 to 2.22) on the PHQ-2, the difference was not statistically significant. Loss of loved ones led to grief (44%), which could be one of the reasons for non-significant outcome in depressive symptoms in the study population. Approximately 4% of residents had an abusive marriage and 4% were abandoned by their family. Perceived lack of social support and grief have been associated with major depressive disorder, which must have played an added role in the persistence of depressive symptoms. [18] Considering the social distancing guidelines that were enforced in the pandemic, loneliness was obvious in residents. Fewer opportunities for sociability and depression were closely correlated in the elderly.[13] Post assessment was delayed due to COVID infection in residents, which could also be responsible for non-significant improvement in depressive symptoms. The structured programme included only one topic/session on depression. Possibly, a greater number of focused sessions on depression may be required to see significant improvement in depressive states. A study on mindfulness and symptoms of depression and anxiety in the general population revealed worry and rumination to be the most significant factors; meditation focusing on reducing worry and rumination may be especially useful in reducing risk of developing clinical depression.[19] Since our study focused on relaxation and meditative exercises, it lacked specific focus on rumination and worry, which might be responsible for non-significant improvement in depressive symptoms. However, the present study did not show any signs of progress in complaints related to suicidal ideation nor increased cases of depressive states or disorder. This may be since all of them were under on-going homoeopathic management before the implementation of programme.
Cognitive impairment did not show much change. Perhaps, no deterioration seen can also be seen as a significant effect of the intervention. Cognitive impairment could be due to structural and/or functional changes occurring with age. Perhaps, a greater number of targeted sessions based on action learning principles is a must to see improvement in symptoms of dementia.
Recovery rate from COVID without complications was relatively higher, probably due to quality care (personal and therapeutic). When 17 out of 24 residents tested positive for COVID, most of the residents experienced distress. However, all of them experienced complete recovery. None of the residents experienced anxiety or depressive symptoms or any distressing mental state and for prolonged period, there was no increment nor deterioration found in their existing complaints as well. A study to assess the effect of COVID-19 on psychological burden of older adults reported increased anxiety and increased depression after acquaintances were infected.[20]
Limitations of the study
Residents during the course of study contacted COVID infection, which delayed the post assessment and might have affected the outcome of study. The number of sessions and modules were pre-defined by HelpAge India, which did not allow to conduct a series of sessions on targeted topics/ symptoms. Perhaps, intervention programmes need to have longer durations to yield lasting results.
CONCLUSION
Anxiety and Depression are commonly found disorders in residents of OAHs. Effectiveness of psychological intervention was significant in alleviating anxiety and helped in restricting the deterioration of depressive states and cognitive impairments. Deeper insights were achieved when dealing with depressive states of residents. These states may need exclusive psychological interventions in longer sessions and series due to presence of deeper emotional trauma and structural changes in the brain responsible for cognitive impairment. However, the structure and process of interventions can be replicated for anxiety-related issues in OAH residents. Execution of a structured programme helped in appreciating the need of a holistic mental well-being programme incorporating a holistic mode of therapeutic intervention like homeopathy.
Acknowledgments
We are grateful to HelpAge India for the financial support. We thank the Trustees of Anand Vruddhashram, Shirgaon, Palghar for agreeing to host the HelpAge mental well-being programme. We thank the Research Department, Dr. M. L. Dhawale Memorial Homoeopathic Institute, Palghar for helping with the statistical analysis.
Recommendations
Homoeopathic management along with psychological interventions should be studied for holistic improvement aiming at efficient coping with depressive states and cognitive impairment for long-term benefits.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
The programme was funded by HelpAge India.
References
- Planning for mental wellbeing in an old age home during the Covid-19 pandemic by homoeopathic institution: Structuring the intervention. J Intgr Stand Homoeopathy. 2021;4:106-11.
- [CrossRef] [Google Scholar]
- Study of psychiatric morbidity among residents of government old age homes in Delhi. J Geriatr Ment Health. 2017;4:36.
- [CrossRef] [Google Scholar]
- COVID-19 pandemic and mental health care of older adults in India. Int Psychogeriatr. 2020;32:1125-7.
- [CrossRef] [PubMed] [Google Scholar]
- Psychiatric and physical morbidity in old age homes of Southern India. IOSR J Dent Med Sci. 2019;18:6-9.
- [Google Scholar]
- Clinical analysis of geriatric patients in the light of homoepathy. Indian J Gerontol. 2016;30:276-83.
- [Google Scholar]
- Demographic and clinical profile of psychiatry patients of rural homoeopathic Hospital, Palghar, Maharashtra, India, from 2014 to 2018. Homœopathic Links. 2021;34:106-11.
- [CrossRef] [Google Scholar]
- Prevalence of psychiatric morbidity amongst the community dwelling rural older adults in Northern India. Indian J Med Res. 2013;138:504-14.
- [Google Scholar]
- Hitting close to home: The effect of COVID-19 illness in the social environment on psychological burden in older adults. Front Psychol. 2021;12:737787.
- [CrossRef] [PubMed] [Google Scholar]
- Reducing Symptoms of Anxiety with Homoeopathic Medicines: A Study Using Small “N” Design. Conference.
- Effectiveness of structured group reminiscence therapy in decreasing the feelings of loneliness, depressive symptoms and anxiety among inmates of a residential home for the elderly in Chittoor district. Int J Community Med Public Health. 2019;6:847.
- [CrossRef] [Google Scholar]
- Homeopathy for dementia. Cochrane Database Syst Rev. 2003;1:CD003803.
- [CrossRef] [PubMed] [Google Scholar]
- An adapted mindfulness intervention for people with dementia in care homes: Feasibility pilot study. Int J Geriatr Psychiatry. 2017;32:e123-31.
- [CrossRef] [PubMed] [Google Scholar]
- Loneliness sociability and depression in old age home elderly. Int J Community Med Public Health. 2019;6:4331.
- [CrossRef] [Google Scholar]
- Depression and Suicide Screening In: Adolescent Health Screening: an Update in the Age of Big Data. Amsterdam, Netherlands: Elsevier; 2019. p. :135-49. Available from: https://www.sciencedirect.com/topics/medicine-anddentistry/patient-health [Last accessed on 2022 Aug 16]
- [CrossRef] [Google Scholar]
- Psychometric properties of the general anxiety disorder 7-item (GAD-7) scale in a heterogeneous psychiatric sample. Front Psychol. 2019;10:1713.
- [CrossRef] [PubMed] [Google Scholar]
- Dementia assessment by rapid test (DART): An Indian screening tool for dementia. J Alzheimers Dis Parkinsonism. 2015;5:3.
- [Google Scholar]
- A biopsychosocial approach to grief, depression, and the role of emotional regulation. Behav Sci. 2021;11:110.
- [CrossRef] [PubMed] [Google Scholar]
- Mindfulness and symptoms of depression and anxiety in the general population: The mediating roles of worry, rumination, reappraisal and suppression. Front Psychol. 2019;10:506.
- [CrossRef] [PubMed] [Google Scholar]
- "Age and ageism in COVID-19": Elderly mental health-care vulnerabilities and needs. Asian J Psychiatry. 2020;51:102154.
- [CrossRef] [PubMed] [Google Scholar]