Translate this page into:
Inpatient department management – An alcoholic man with acute exacerbation of pancreatitis
*Corresponding author: Sonam Ashishkumar Tiwari Mishra, Assistant Professor, Department of Medicine, Dr. M. L. Dhawale Memorial Homoeopathic Institute, Palghar, Maharashtra, India. sonam.a.tiwari@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jain BS, Mishra SA. Inpatient department management – An alcoholic man with acute exacerbation of pancreatitis. J Intgr Stand Homoeopathy 2020;3(2):51-6.
Abstract
Alcoholism of long standing is the major cause of acute pancreatitis. Ethanol is well recognized as a chemical toxin, but a significant injurious effect on pancreatic acinar or duct cells has yet to be demonstrated. It also stimulates secretion from small intestine, which triggers the exocrine pancreas to release pancreatic juice. When these effects occur together the results may be disastrous. Homoeopathic management needs accurate data collection, to exact assessment of the state and stage of disease with awareness of developing complications. Arriving at exact simillimum in acute state with definition of susceptibility and assessment of remedy response needs close observation and monitoring. Having an inpatient department set up manned by PG student is an asset for this management. Case study demonstrates this effort by the team.
Keywords
Acute exacerbation of pancreatitis
Addictions
Posology
Challenges in inpatient department
INTRODUCTION
Pancreatitis, whether acute or chronic, is an emergency that is almost always painful and often fatal. Use of alcohol is a worldwide habit regardless of socioeconomic background. Heavy alcohol consumption is a potential risk factor for induction of pancreatitis.[1] Acute pancreatitis secondary to alcohol is more common in men, whereas gallstone-related pancreatitis is more common in women.[2] Acute pancreatitis should be treated as early as possible to avoid complications.
If homoeopathy is selected in cases of acute pancreatitis, quick hospitalization with proper homoeopathic case taking is essential for treatment as it enables the physician to determine the simillimum. Homoeopathy can play an important role in relieving the acute inflammation as the prescription is based on a study of the susceptibility and miasm. Acute case taking is always a challenge in the emergency state. Quality data collection and quick assessment of the clinical state and susceptibility goes a long way in treating these cases and preventing further complications[Table 1]. Homoeopathy can offer this, with the added benefit of being a mild form of treatment.
| Local | Systemic |
|---|---|
| Pancreatic fluid collections, pancreatic abscess, pancreatic pseudocyst | Pulmonary: Pleural effusion, pneumonitis, adult respiratory distress syndrome |
| Pain, rupture, hemorrhage, infection | Cardiovascular: Hypotension, hypovolemia, nonspecific ST-T changes in electrocardiogram simulating myocardial infarction, pericardial effusion |
| Obstruction of the gastrointestinal tract (stomach, duodenum, colon) | Hematologic: Disseminated intravascular coagulation |
| Disruption of the main pancreatic duct Involvement of contiguous organs due to necrotizing pancreatitis | Gastrointestinal hemorrhage: Erosive gastritis, hemorrhagic pancreatic necrosis with erosion[5] |
Pathogenesis
In acute alcoholic pancreatitis, there is precipitation of protein plugs, which serve as niduses for subsequent calculi obstructing the ductal system. Early pancreatitis features hypersecretion of enzyme proteins by the acinar cells, without concomitantly increased fluid. Due to this, protein plugs precipitate in the small branches of the pancreatic ducts, which then enlarge to form laminar aggregates through accretion of amorphous material. Repeated episodes of necroinflammation may trigger the activation of pancreatic stellate cells, which are usually inactive in the normal pancreas.[3]
Clinical features
Abdominal pain located in the epigastrium and periumbilical region, radiating to the back and lower abdomen, along with nausea, vomiting, and abdominal distention.[3]
Physical examination
Hypotension, tachycardia, and low-grade fever with jaundice. Pulmonary findings: Basilar rales, pleural effusion (left-sided). Abdominal tenderness and muscle rigidity present. Bowel sounds: Diminished or absent. Positive Cullen’s sign and Turner’s sign indicate severe necrotizing pancreatitis.[4]
Complications
Investigation findings
Leukocytosis (15,000–20,000 g/l), hyperglycemia, abnormal liver function test with raised lactate dehydrogenase levels (>8.5 mol/L), serum lipase, and amylase levels 3 times the normal.[5]
Essential imaging studies
Ultrasound examination may demonstrate the underlying cause, for example, gallstones or pancreatic calcification, as evidence of pre-existent chronic pancreatitis.
Contrast-enhanced computed tomography is an essential tool for determining the presence and extent of necrosis.
Magnetic resonance cholangiopancreatography allows proper visualization of pancreatic and biliary duct anatomy.
CRITERIA TO ASSESS THE SEVERITY OF ACUTE ALCOHOLIC PANCREATITIS
Severity of pancreatitis is measured with one or more of the following scales:
The bedside index of severity in acute pancreatitis (BISAP):[6] (1) BUN >25 mg/dL (1 point), (2) Glasgow coma scale score <15 (1 point), (3) evidence of systemic inflammatory response syndrome (1 point), (4) patient age >60 years (1 point), and (5) imaging study reveals pleural effusion (1 point)
The Ranson criteria[5]
The APACHE II score.[5]
CASE
Background information
The patient had initially reported to the casualty ward of the hospital on 20-07-13 (4.35 pm). The chief complaint was epigastric pain for 7–8 days with tightness of abdomen and sour eructation. The stool was watery, sticky, and occasionally blackish. On arrival, the patient had not passed stool for 2 days. He had nausea with 1 episode of vomiting and occasional mild cough with white sticky expectoration for 2 days. As the patient was not willing for admission, an injectable (antispasmodic) was administered and the patient went home.
On 21-07-13 (1.30 am), the patient returned to the casualty ward with the same complaints, but the intensity had increased.
Condition of the patient during admission
The patient reported considerable weakness due to nausea and vomiting. His pain was so intense that he was unable to eat anything and was forced to report to the casualty ward at 1.30 am. On examination, his vitals were stable. Random blood glucose level was 108 mg/ dL. Per abdomen examination yielded severe epigastric tenderness with rigidity; bowel sounds sluggish but present all over.
The patient and his relatives were reassured and oriented for homoeopathic treatment, after which the patient was admitted to the inpatient department (IPD).
Preliminary data
Name: Mr. R K
Age: 32 years
Sex: Male
Date of case taking: 21-07-13
IPD no A – 256/ B – 2554.
Chief complaint:[7] Chief complaint is written in the LSMC format for better clarity [Table 2]
| Location | Sensation | Modalities | Concomitants |
|---|---|---|---|
| Gastro intestinal tract | Pain cramping+3 | >Pressure+3 | Irritability+2 |
| Pancreas | Nausea+2 | <Lying on left side+3 | Thirst |
| Epigastric region to Back | Vomiting- scanty, sticky, non- offensive, non-projectile, no hematemesis | >Lying on right side+2 | reduced+3 |
| Anus | Stool- character changeable, watery- semi-solid- hard, mucous, sticky, blackish, reddish. | <Bending forward+2 | Sleep |
| Onset: sudden | burning+2 | <Vomiting after+2 | disturbed+2 |
| Duration: 7–8 days | <During stools+1 | ||
| Progress: Progressive | <After stools+1 | ||
| Frequency: Variable | |||
| Intensity: Variable |
Addictions
Alcoholic for 15 years, consumption upto 1 litre/day (4–5 times/week); chronic smoker (1 packet daily) for 15 years.
Medical history
Acute hepatitis, cholelithiasis, and chronic pancreatitis admitted in tertiary hospital with similar complaints 6 months earlier.
General examination
Vitals: Stable.
Systemic examination
Per abdomen: Epigastric tenderness with rigidity. Percussion: tympanic note. Bowel sounds: sluggish in all quadrants.
Bowel sounds: Diminished or absent due to gastric and transverse colonic ileus.
Rigidity: Involuntary response to prevent pain more pronounced in the upper abdomen.
Rest normal.
Investigations: (21-07-13)
Hemoglobin: 15.4 g/dl, total WBC count – 10,500 g/dl, platelets: Adequate; serum creatinine: 0.58 mg/dL, BUN: 7.7 mg/dL, bilirubin (total): 0.73 mg/dL, bilirubin (indirect): 0.30 mg/dL, SGOT – 52.5 U/L, SGPT – 33.6 U/L, serum amylase: 435 U/L, and serum lipase: 450 U/L.
USG abdomen: (22-07-13): Bulky pancreatic duct 3 mm, gallbladder 6 mm polyp.
The BISAP assessment: Treatment started in an early phase, considering the history of repeated episodes of pancreatitis. Therefore, the patient had a lower chance of developing complications.
On the basis of available signs and symptoms, the BISAP criteria were found most suitable for the assessment.
Probable diagnosis with understanding
The severity of pain with back radiation and associated features of nausea and vomiting with a history of recurrent episodes is highly suggestive of acute exacerbation of chronic pancreatitis. The history of alcohol abuse helped confirm the diagnosis. The investigation results, including the elevated serum lipase and amylase levels along with the ultrasonography findings favor acute pancreatitis.
Diagnostic criteria of acute exacerbation of alcoholic pancreatitis
The history of alcohol abuse with evidence of acute abdominal pain radiating to the back, raised serum amylase and lipase levels over 3 times the normal, and investigation findings suggest injury to the pancreas.
Stage of Pathology: Structural reversible disease
Totality:[8] (Boger approach)
Time, pathogenesis (location and pathology), sensation, physical general, modalities, and mental state [Figure 1].
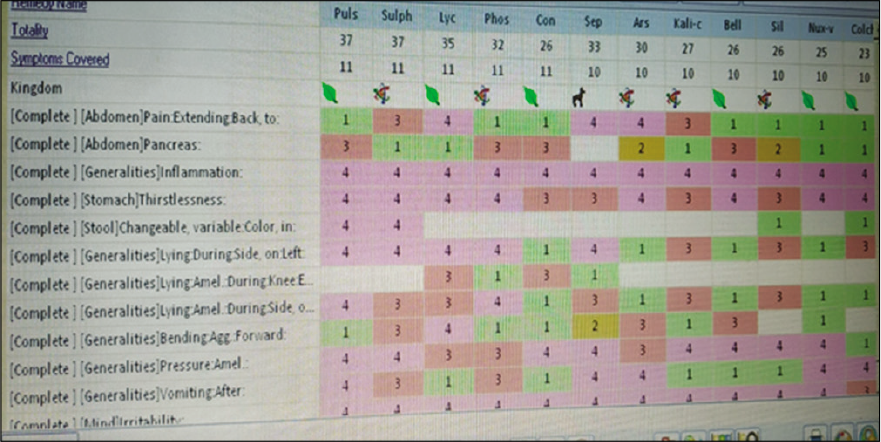
- Repertorial totality of the case
Acute exacerbation- pace- moderate
Abdomen - direction backward2+
Pancreas, glands
Colon
Inflammation – necrosis
Pain cramping
Burning
Thirstlessness3+
Discharge: Diarrhea changeable
<Lying on left side+2
<Bending forward+2
>Pressure+3
>Lying on right side+2
<Vomiting after2+
Irritable+2.
Remedy differentiation: Pulsatilla/Nux Vomica/Phosphorus [Table 3]
| Topics | Pulsatilla N | Nux vomica | Phosphorus |
|---|---|---|---|
| Sphere of action | Mucous membrane-stomach, bowels, glands | Digestive system-stomach, liver, bowels | Mucous-membranes-stomach, lungs, liver |
| Abdomen | Thirstlessness with nearly all complaints Epigastrium- cutting pulsation heavy or deranged stomach Stool- changeable Abdomen as heavy as of a stone, aching, pain radiating to the groin |
Bruised soreness of abdomen, fainting after vomiting, after stool Gastric pains into back, > vomiting Nausea > if he can only vomit |
Thirst unquenchable for large quantity of cold water Sour taste, eructation, regurgitation Craving for cold drinks, > but vomited out empty hollow feeling and sore spot in epigastrium |
| Modalities | <Warmth of air, <lying on left side, rich foods >cold, >continued motion, >pressure, >changing sides | <Cold- open air, uncovering, liquor, over eating, <slight cause- pressure, touch | <Lying on left side, <cold air >eating, sleepsitting up, rubbing[9,10] |
Pulsatilla was selected as the final remedy considering the underlying pathology (glands, organs, and tissues), characteristic physical generals,[9] and characteristic modalities as presented in the above table.[10]
Planning and programming:[11]
Potency selected was 200 as per the patient’s susceptibility assessed through planning and programming [Table 4].
| State | Potency | Repetition |
|---|---|---|
| Susceptibility (Tissue) onset- sudden Progress- progressive Pathology- structural reversible Symptoms- characteristic physical particular acute disease on chronic |
30 | frequent |
| Sensitivity (mind and nerves) mind+, nerves+3 | 200 | Infrequent |
| Structural changes- reversible | 30 | Frequent |
| General vitality- good | 200 | Frequent |
Final remedy: Pulsatilla Nigricans Susceptibility: Moderate – Potency: 200
Follow-up criteria
Details are shown in [Table 5].
| No | Subjective symptoms | Objective symptoms |
|---|---|---|
| 1 | Thirst | General condition |
| 2 | Sleep | AG |
| 3 | Epigastric pain | Pulse rate |
| 4 | Nausea | Blood pressure |
| 5 | Vomiting | P/a examination- look for bowel sounds, tenderness, rigidity |
The bedside index of severity in acute pancreatitis score assessment
Remedy reaction
The patient was better with Pulsatilla 200, which signifies that remedy registration was seen but the potency was insufficient as pain and sleep were not improving further. Therefore, the potency was increased to 1 M, which resulted in a complete cure. The resident surgeon also examined the patient and advised continuing the ongoing line of treatment [Table 6].
| Date | Treatment | Subjective symptom | Objective symptom | Action taken | Interpretation |
|---|---|---|---|---|---|
| 21-7-13 | Pulsatilla 200 | Nil by mouth, Intravenous fluids, wait and watch | |||
| 3.15 am | 2 hourly | - | - | ||
| 21-07-13 | Pulsatilla 200 | 1. Increased | 1. Improved | Nil by mouth, intravenous fluids, continue same treatment wait and watch | Medicine registration seen |
| 7 am-7.00 pm | 2 hourly | 2. SQ | 2. 91 cm | ||
| 3. SQ | 3. 72–78/min | ||||
| 4. 0 | 4. 120–80 mmHg | ||||
| 5. 0 | 5. Tenderness: Present (epigastric region) with rigidity | ||||
| Bowel sounds: Sluggish in all quadrants | |||||
| 21-07-13 | Pulsatilla 1M 2 | Same as above | Same as above | Increased the potency | Thirst improved no nausea and vomiting. Sleep disturbed due to pain |
| 11.00 pm | hourly | ||||
| 22-07-13 | Pulsatilla 1M 2 hourly | 1. Improved | 1. Improved | Surgical opinion taken, advised to continue same treatment | Patient improving |
| 7.00 am-7.00 pm | 2. Improved | 2. 90 cm | |||
| 3. >60% | 3. 74–80/min | ||||
| 4. 0 | 4. 120–80 mmHg | ||||
| 5. 0 | 5. Bowel sounds- present, mild tenderness, no rigidity | ||||
| 23-07-13 | Pulsatilla 1M 2 hourly | 1. Improved | 1. Improved | All complaints better vitals stable | |
| 2. Improved | 2. 87.5 cm | ||||
| 3. >80 % | 3. 74–80/min | ||||
| 4. 0 | 6. 120–80 mmHg | ||||
| 5. 0 | 7. Bowel sounds- present, no tenderness, no rigidity |
The bedside index of severity in acute pancreatitis assessment score – 0 (LOW MORTALITY)
Investigations before and after treatment
On the day of discharge, the patient was tolerating soft diet well. His vitals were stable. On 23-07-13, the patient was sent to Mumbai for endoscopy (further workup). He was advised to follow-up in the OPD with the endoscopy reports for further management.
CONCLUSION
Homoeopathy has a good scope in treating acute exacerbation of alcoholic pancreatitis
Management requires quick assessment of clinical state, stage, and possible complications
Management needs quick case taking to unearth the characteristics as well as assessment of the clinicopathological stage through investigation and examination
Assessment of susceptibility is essential to decide posology and monitor the remedy regulation and outcome
All the above factors help the homoeopath determine the correct indicated remedy
The correct homoeopathic remedy can bring about fast recovery without complications.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Pathophysiology of acute pancreatitis: An overview. World J Gastroenterol. 2006;12:7421-7.
- [CrossRef] [PubMed] [Google Scholar]
- The pancreas In: Sternberg’s Diagnostic Surgical Pathology (5th ed). Philadelphia, PA: Lippincott Williams and Wilkins; 2010.
- [Google Scholar]
- Exocrine pancreas In: Townsend CR, Beauchamp DR, Evers M, Mattox K, eds. Sabiston’s Textbook of Surgery (19th ed). Philadelphia, PA: Saunders, Elsevier Inc.; 2012.
- [Google Scholar]
- Hepatobiliary and pancreatic diseases In: API Textbook of Medicine (6th ed). Mumbai: Association of Physicians of India; 1999.
- [Google Scholar]
- Acute and chronic pancreatitis In: Harrison’s Principles of Internal Medicine (17th ed). United States: The McGraw-Hill Companies; 2008.
- [Google Scholar]
- Bedside Index of Severity in Acute Pancreatitis (BISAP Score) 2020. Available from: https://www.merckmanuals.com/medical-calculators/bisapscore.htm [Last accessed on 2020 Apr 04]
- [Google Scholar]
- The Art and the Science of Standardized Homoeopathic Practice, Education and Training, Step-1, Case Summary, Chief Complaint, Mumbai.
- [Google Scholar]
- Perceiving scientific method: Repertorisation, standardization In: D2-Repertorial Concept and Technique (3rd ed). Mumbai: Dr. M. L. Dhawale Memorial Trust; 2003.
- [Google Scholar]
- Pocket Manual of Homoeopathic Materia Medica (9th ed). New Delhi: Mayur Jain, Indian Books and Periodicals Publishers; 2007.
- [Google Scholar]
- Principles and Practice of Homoeopathy (4th ed). Mumbai: Dr. M. L. Dhawale Memorial Trust; 2006.
- [Google Scholar]